The novel coronavirus, severe acute respiratory coronavirus 2 (SARS-CoV-2), is the pathogen responsible for chronic coronavirus disease 2019 (COVID-19). Approximately 20–55% of COVID-19 patients are reported to be hospitalized with deranged hemostatic laboratory parameters, suggesting coagulopathy.
These anomalies include a slightly prolonged prothrombin time (PT), higher D-dimer density, mild thrombocytopenia, and, in advanced stages, decreased fibrinogen. Studies suggest that high concentration of D-dimer is associated with adverse clinical outcomes, such as the need for intensive care or even death. The available data indicate that COVID-19 is characterized by a pro-thrombotic state driven by massive thromboinflammation, possibly arising from diseased lung endothelial cells.
A better understanding of COVID-19-related coagulopathy is critical for health care practitioners to reduce the risk of thrombosis and bleeding by throwing out treatment options.
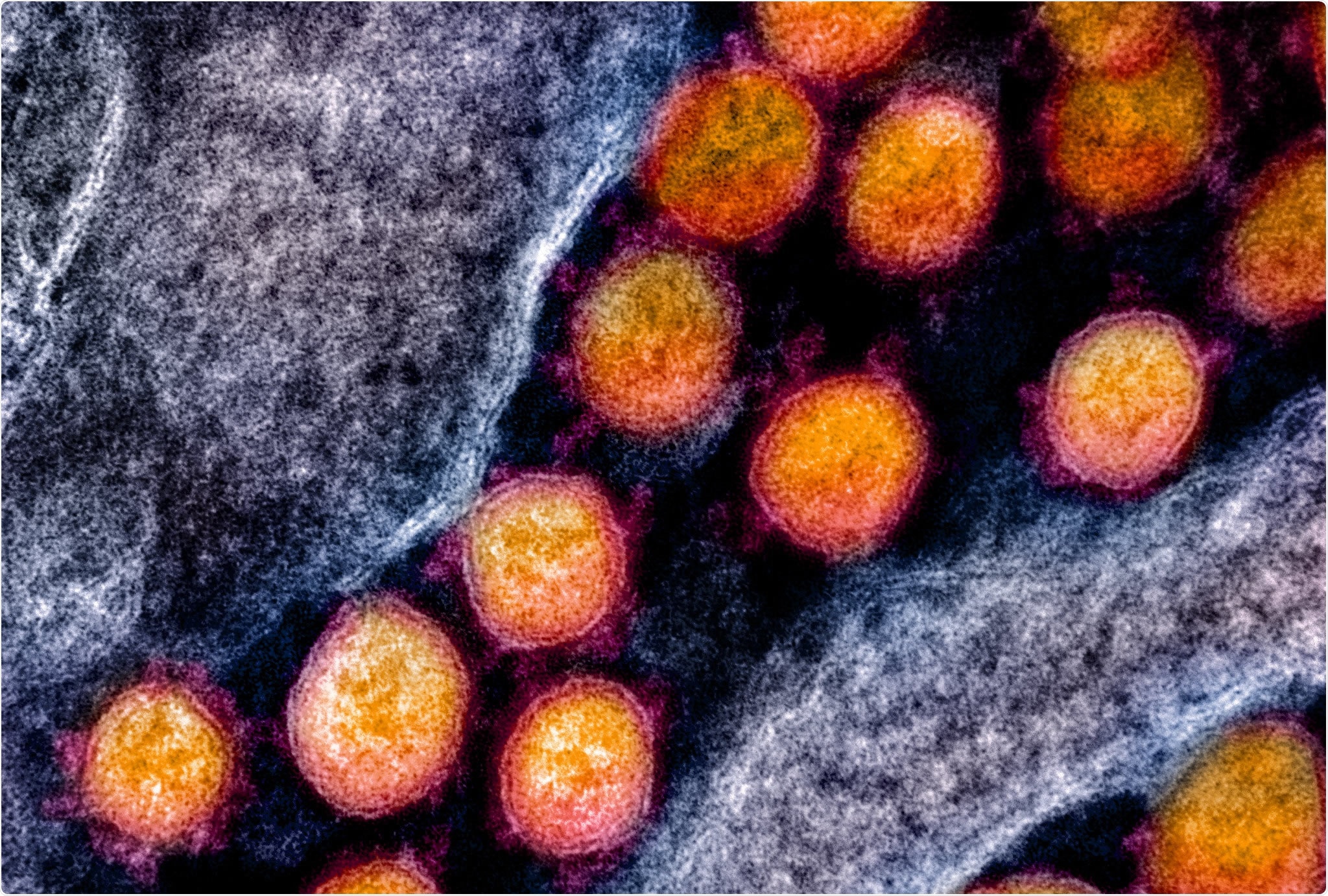
Transmission electron micrograph of SARS-CoV-2 virus granules, isolated from patient. Image captured and enhanced by color at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Systematic review of the association between hemostatic parameters and adverse effects of COVID-19
Recently, a team of researchers from Canada and the US routinely demonstrated the association between hemostatic laboratory parameters and key clinical outcomes among adult COVID-19 patients. They analyzed hemostatic parameters such as PT and D-dimer density in COVID-19 patients and their association with clinically important outcomes such as bleeding, thrombosis, true disease, and mortality. The review is published on the preprint server, medRxiv*.
The team conducted a systematic review of observational studies, randomized clinical trials, and case series published in PubMed (Medline), CENTRAL, and EMBASE between December 1, 2019, and March 25, 2020. Studies of COVID- adult patients 19 who reported at least one hemostatic lab parameter was included in the study.
Elevated D-dimer concentration is the strongest predictor of clinical adverse effects
The researchers extracted data from 57 studies, including more than 12,000 patients who met their inclusion criteria. 45% of the patients in the studies were women, and the average age of patients was 52 years. Of the studies included in the review, 92.7% (N = 38/41) of studies reported an average platelet count greater than 150 x 109/ L, 68.2% (N = 15/22) of studies reported an average PT of 11 – 14 s, 55% (N = 11/20) of studies reported an average activated partial thromboplastin time (aPTT) in the range de
25 – 35 s, and 34.4% (N = 11/32) of studies reported D-dimer density above the maximum of normal (ULN).
Eight studies, including 7 peers and 1 case series, reported hemostatic lab values for survivors vs non-survivors. D-dimer density was reported in 4 studies among non-survivors, all of whom reported an average D-dimer level above the ULN.
Based on the findings, the researchers concluded that the majority of COVID-19 patients were hospitalized with normal platelet count, PT and aPTT values in the high referral interval, and increased density. D-dimer. However, there was no explanation for how these hemostatic parameters were associated with adverse outcomes. D-dimer elevation appeared to be the strongest predictor of clinical adverse effects.
“COVID-19-associated coagulopathy has been thought to be mediated by pulmonary vascular endotheliopathy, which may increase the risk of thromboembolism and death in hospitalized patients with COVID-19. ”
The findings could help physicians try COVID-19 patients with coagulopathy
The authors believe that these results provide a framework for managing HCPs that care for COVID-19 patients. The results agree with data from COVID-19 patients in the hospital in Wuhan, China, which showed a moderate D-dimer concentration of 2.4 mg / L in patients requiring emergency care compared to 0.5 mg / L in those that did not require emergency care.
Similarly, a study in New York reported that 4-fold higher D-dimer density was associated with approximately 5-fold higher incidence of disease severity compared to normal D-dimer density.
This information may help physicians diagnose COVID-19 patients with coagulopathy and support the recommendation to closely monitor patients within COVID-19 with elevated D-dimer concentration. According to the authors, further studies are necessary to confirm this correlation between hemostatic parameters and the risk of adverse clinical outcomes such as bleeding and thrombosis.
“This information will assist facial health practitioners in the use of hemostatic laboratory parameters for prognostication as well as in testing patients to the appropriate condition, which is especially critical in the case of a pandemic if resources dwindle. ”
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.
Magazine Reference:
- Coronavirus-19 and coagulopathy: A systematic review [COVID-COAG], Stephanie G Lee, Michael Fralick, Grace Tang, Brandon Tse, Lisa Baumann Kreuziger, Mary Cushman, Peter Juni, Michelle Sholzberg, medRxiv 2021.01.05.20248202; doi: https://doi.org/10.1101/2021.01.05.20248202, https://www.medrxiv.org/content/10.1101/2021.01.05.20248202v1