
The 2019 pandemic of coronavirus infection (COVID-19) has resulted in more than 2.15 million deaths, among more than one hundred million recorded cases of infection with the causative agent, coronavirus respiratory syndrome 2 (SARS-CoV-2). About eight out of ten have died in the elderly, making up just a tenth of all cases.
A new introduction appears on the medRxiv * server describes the changes that occur in several antibodies and inflammatory molecules with age and at different stages, or the severity of the disease and the resulting disease. The results may help to predict the risk in individual cases.
The gold standard for the diagnosis of SARS-CoV-2 disease is by transversease-polymerase chain test (RT PCR), using nasopharyngeal swabs (NP), oropharyngeal swabs (OP), nasal swabs, or saliva, usually within five days. of tonight. In most cases, symptoms begin within five days of onset.
The current study evaluates the use of antibody tests to detect the infection, possible immunity, and detect cases within a home where an outbreak or recorded infection has occurred.
In PCR-positive individuals, Immunoglobulin M (IgM) antibodies appear within the middle of five days from the earliest symptom and last with time. Immunoglobulin G (IgG) and neutral antibodies appear in the middle 14 days after the onset of the symptom and last for months.
Antibody levels increase with age
The study used IgG values from samples obtained from more than 79,000 subjects and IgM levels from approximately 62,000 of them. Approximately 5% and 3% were positive for IgG and IgM, respectively, with moderate IgG titers of 44 AU / mL, 1010 AU / mL, and 1111 AU / mL in individuals younger than 45 years. , 45–64, and 65 years or older, respectively. This indicates that titers are more than twice as high in the two older strata compared to the younger ones, both for males and females. However, males had higher IgG levels than females in the 45-64-year-old age group.
Second, IgM titers were more likely to be detected in women over 65 years of age than in the youngest age group.
Antibodies in meat packaging workers
Of the ~ 350 meat packing plant workers tested, IgG postage occurred in nearly one-fifth (19%), and IgM postage occurred in 1515%. At another center, of 217 employees tested, a quarter (51 people) were positive with PCR. The majority (75%) of the 41 PCR-positive relapses two weeks later remained positive.
At this stage, 711 71% and 1010% showed seroconversion for IgG and IgM, respectively. Nearly two thirds reported a symbolic disease. The median IgG and IgM values in the 41 patients diagnosed at two weeks of infection were 20.5 and 0.5 AU / mL, respectively, but the IgG titers varied over a wide range.
Interestingly, 25 PCR-negative individuals who requested antibody tests had positive IgG and IgM levels, respectively, because of their symptoms and exposure history. Everyone who was positive for IgM had persistent symptoms. Median titers for IgM and IgG in these individuals were 2525 and 1 AU / mL, respectively.
“These data clearly document the benefits of antibody testing for case detection in previously exposed subjects even with negative RNA tests. ”
Antibodies in healthcare provider’s office settings
At one health care provider’s office in the Bronx, New York, nearly 290 patients were tested for antibodies. Approximately 18% and 5% had positive and marginal IgG values. Symptoms were reported in six of ten patients in the border group, with three with a history of PCR imaging, and six of whom had been exposed to the virus.
Antibodies in family collections
The researchers found that when PCR and antibody positivity were compared in 154 outpatients, 22 individuals (1414%) were positive for both. Seven of these were followed, by their families, and nine advanced people, many with apparently symptomatic symptoms. Three of his followers, all over 80, needed to be admitted to hospital, two were admitted for ventilation, and one died.
The data showed that antibody testing could identify additional issues in family collections, that PCR prophylaxis could last up to six weeks, and that IgM levels could be elevated for long periods in patients with symbolic chronic illness.
Antibodies and inflammatory molecules in PCR assays
The researchers also compared antibodies (IgM, IgG, and neutralizing antibodies) and specific inflammatory markers (IL-6, hsCRP, and ferritin) between PCR negatives and two groups of positive PCR factors (outpatients and side patients). inside). They found that all controls were antibody negative.
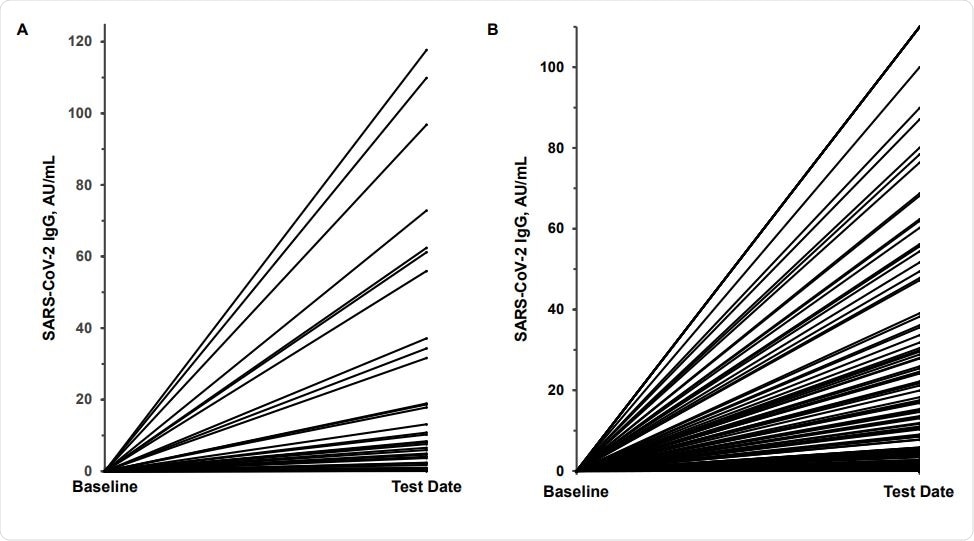
PCR-positive had higher 300-fold and 600-fold moderate IgG titers in outpatients and patients, respectively, compared with controls. Again, there was a wide variation between individual patients (1–200 AU / mL and 0.05 to 170 AU / mL, in outpatients and inpatients, respectively.
IgM values also showed higher two- and five-fold values in outpatients and inpatients compared to controls. Medium-term 12-fold and 24-fold higher-dose antibodies were also present in outpatients and inpatients, respectively. These two groups differed significantly from about 1–14 AU / mL in outpatients and 0.5–19 AU / mL in inpatients, respectively.
The data show significantly higher antibody titers in advanced PCR items than controls.
With IL-6, median titers in controls did not differ from those in outpatients, but patients titers were 75 times higher compared to other groups. However, the range of individual titles expanded from 0.75-5500 pg / mL. The same pattern was observed with hs-CRP, with 80-fold higher middle titers, and ferritin with nine-fold higher middle titers.
If the hs-CRP cutoff was 10 mg / L or more, 93% of inpatients, but only 6% of controls or outpatients, would have positive tests. The researchers suggest that being PCR-positive, with hs-CRP values above this threshold, had a 17 times higher risk of seeking hospitalization than hs-CRP values below this level. , making it a useful predictor of the severity of disease.
Algorithm for hospital risk
The researchers developed a new algorithm to predict patients who needed to go to the hospital. They used IL-6, hs-CRP, and IgM as markers, all as part of the ‘cytokine storm’ associated with severe COVID-19, with thresholds of ≥10 pg / mL ≥10 mg / L, and ≥1.0 AU / mL, respectively. They found that increases in these molecules predicted hospitalization in 8686%, 6060%, and 1212% of patients.
If two or more of these were elevated, nearly 98% would be hospitalized, but only 2% of the others, presenting a 50-fold risk in this group. IgG, neutralizing antibody, and ferritin were excluded as they did not further increase the value of the model.
What is the impact?
The study shows a double-digit antibody titer in elderly patients. In addition, they found that antibody testing is useful in identifying cases, as well as monitoring antibody levels in convalescent plasma (CP).
The researchers also found very high variability in antibody titers in PCR-positive patients. If the IgG threshold is set above> 6.5 AU / mL (1: 320, according to FDA guidelines), only half of patients would be PCR positive. One-third would have rates> 20 AU / mL (> 1: 1000).
IgG levels are closely linked to neutralizing antibody levels. And finally, when two or more of the IL-6 ≥10 pg / mL, hs-CRP ≥10.0 mg / L, and / or IgM ≥1.0 AU / mL signals are present, it is very likely to be necessary. at the hospitalized patient.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.