.jpg)
Acute respiratory coronavirus 2 (SARS-CoV-2) syndrome, the virus that causes the coronavirus infection (COVID-19), causes a wide range of symptoms outside the respiratory tract.
Many patients report many symptoms that affect the cardiovascular system and the nervous system. There is growing evidence that SARS-CoV-2 disease can lead to long-term neuropsychological deficits, even in its mild or moderate respiratory forms.
A team of researchers at the Clinical and Experimental Neuropsychology Laboratory, Faculty of Psychology, University of Geneva, Switzerland, reports that SARS-CoV-2 may affect the central nervous system, especially the system limbic which is dependent on behavioral and emotional responses.
The study, published in the pre-print service medRxiv *, showing long-term neuropsychological sequelae after COVID-19, regardless of the severity of the respiratory disease.
Study background
Health experts have suspected long-term neuropsychological deficits following SARS-C0V-2 infection. For example, previous studies of the two previous coronary fractures, severe respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS), have shown neuropsychological symptoms such as sleep disorders, emotional weakness, anxiety disorder, frequent traumatic memory. experiences, memory loss, and fatigue in over 15 percent of affected patients approximately one month to 3.5 years after infection.
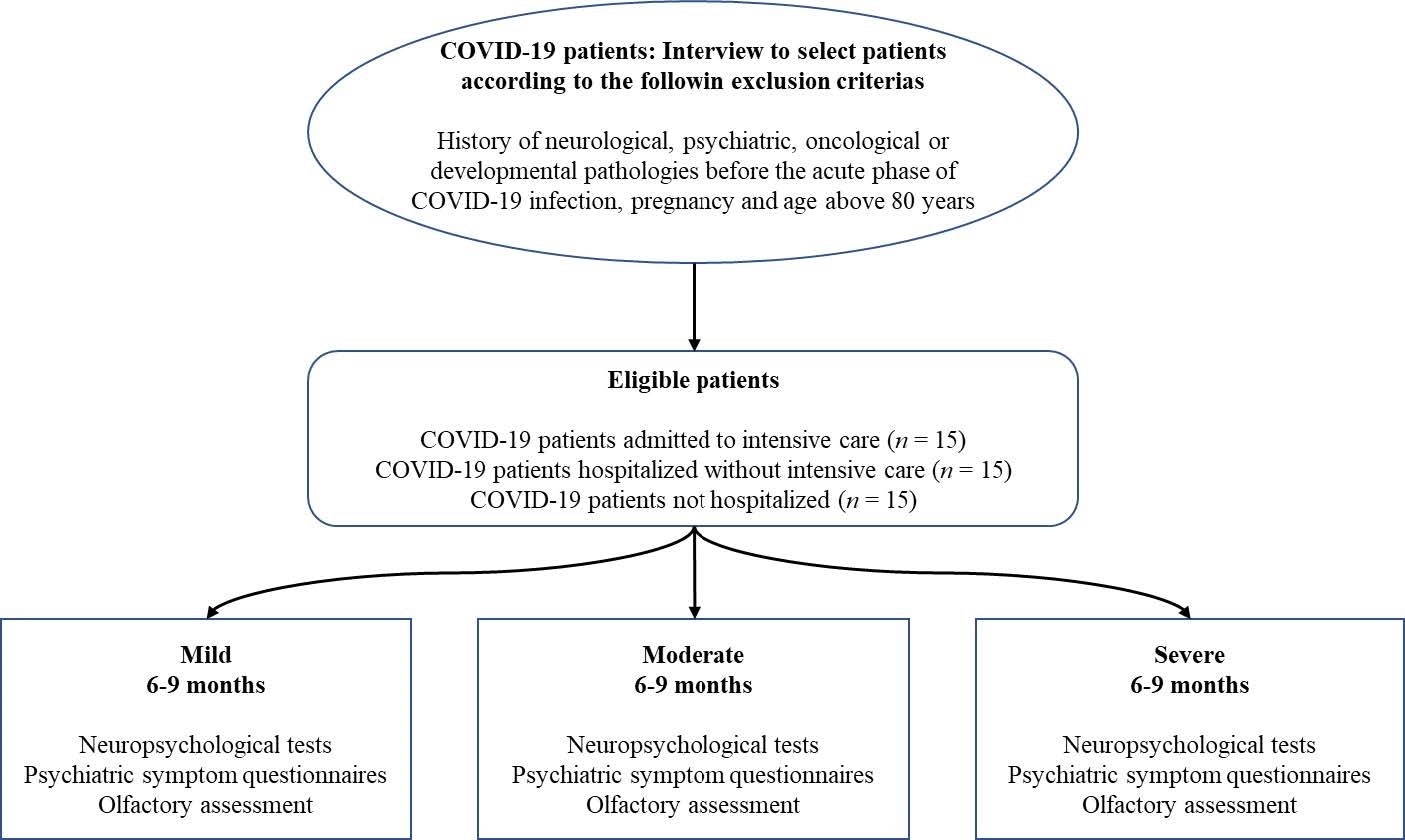
Study flowchart
Furthermore, in other diseases such as the Human Immunodeficiency Virus (HIV), encephalitis, and multiple sclerosis, studies have revealed specific long-term deficits in mental functions, including emotional and memory responses,
In COVID-19, however, there are reports of increased stroke in patients, leading to short- and long-term neurological and cognitive deficits. Finally, sudden onset of anosmia or loss of smell was indicated as a symptom in COVID-19 patients.
This symptom occurs because olfactory epithelium carries angiotensin-converting enzyme 2 (ACE2) receptors, the cellular gateway that the virus uses to enter human cells. Scientists proved that the virus may have used a nasal brain barrier to get into a virus.
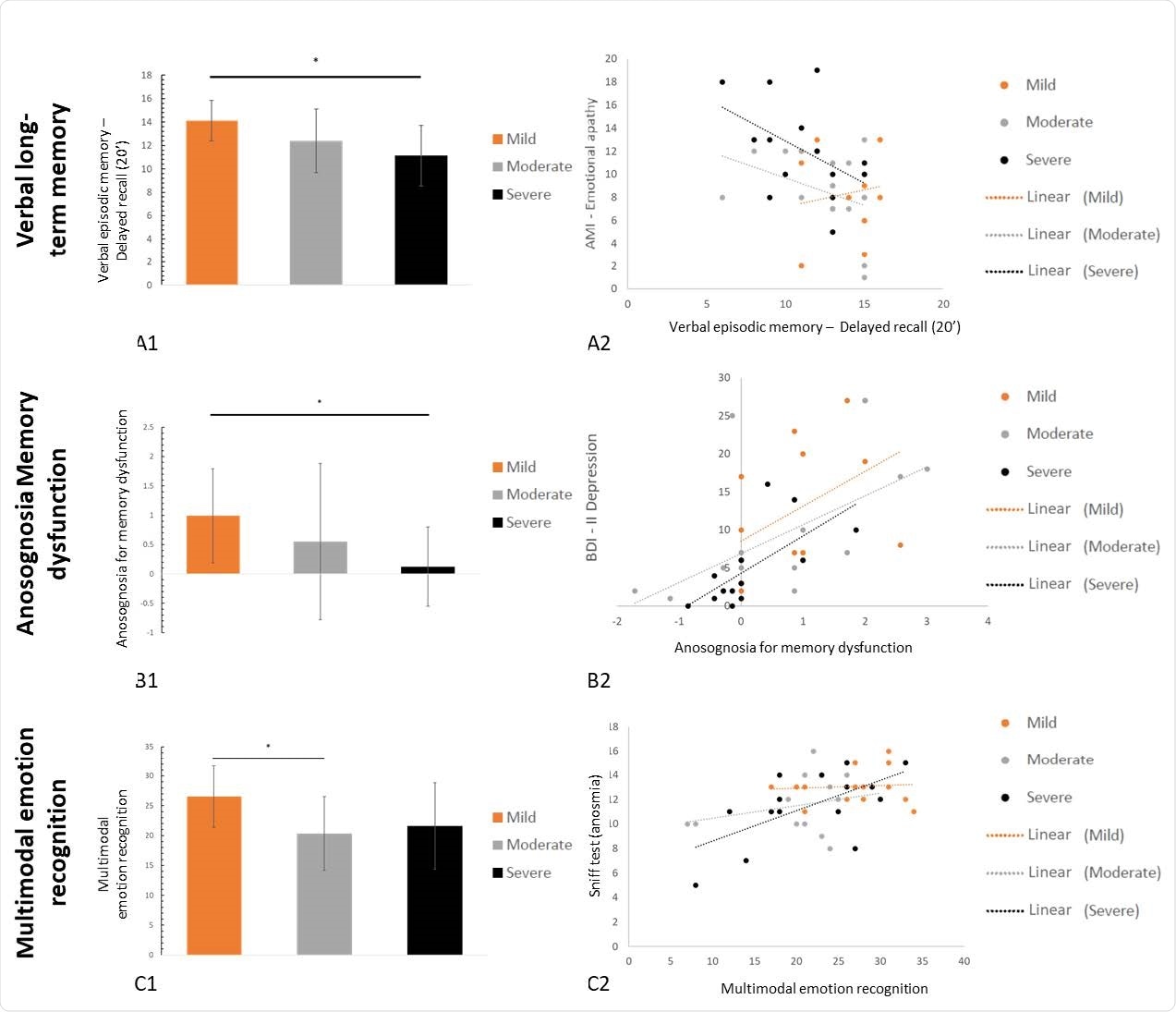
Average levels (and normal movements) for all three groups (hard in black, medium in gray, and mild in orange) on activities evaluating verbal episodic memory (A1), anosognosia for memory dysfunction (B1), and recognition multifactorial emotion (C1), as well as the individual predictors (A2, B2 and C2).
The study
The current study aims to determine the effect of SARS-CoV-2 infection on the brain. The team wants to study whether COVID-19 causes long-term neuropsychological deficits from 6 to 9 months, identify the nature of the affected areas, and experience the impact of these deficiencies on the quality of life of the patients.
The team administered neuropsychological, neurological, psychiatric, and olfactory tests to 45 patients to reach the conclusions of the study.
The team divided the patients into three groups, depending on the severity of the respiratory infection in the acute stage: severe, moderate or moderate. Adverse cases were admitted to the intensive care unit with respiratory support, moderate cases were admitted to the hospital without respiratory support, and mild patients were not admitted to the hospital.
The researchers found a high frequency of psychiatric symptoms, regardless of the severity of the disease, in the acute stage of the disease. Patients in all three groups showed symptoms of depression, mania, anxiety, stress, apathy, post-traumatic stress disorder (PTSD), and dissociative disorders. Some patients reported insomnia, fatigue, and pathological somnolence.
When it comes to odor perception, 33.33 percent of the mild group, 73.33 percent of the middle group, and 46.66 percent of the hard group or partial loss of smell six to nine months after being infected have hyposmia. Meanwhile, of the hardy group, anosmia was still at 13.33 percent or total odor loss.
Although the reported mental deficits in all three groups were common, some areas of mental and emotional affect were different, depending on the severity of the disease. In long-term episodic memory, the patients performed a worse group worse than the mild group. They also showed increased anosognosia for memory loss.
At the same time, the mild group had more stress, anxiety, depression, and reported more interesting issues. The middle group recognized multifactorial emotions as well as the mild group. All of these manifestations have affected the lives of the patients.
“At this stage, it is difficult to determine whether the mental deficits can be considered a sign of brain damage and / or whether they should be linked to psychosocial variables that may themselves be directly caused by them. from diseases with SARS-CoV-2 or other induced by the severity of the generalized pandemic and the individual experience of the disease, ”the researchers explained.
The team recommends that clinical guidelines and recommendations be implemented in the management of long-term brain disorders following SARS-CoV-2 infection.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.
Magazine Reference:
- Prolonged neuropsychological complications of COVID after severe, moderate or mild disease, P. Voruz, G. Allali, L. Benzakour, A. Nuber-Champier, M. Thomasson, I. Jacot, J. Pierce, P. Lalive, KO. Lövblad, O. Braillard, M. Coen, J. Serratrice, J. Pugin, R. Ptak, I. Guessous, BN Landis, F. Assal, JA Péron, medRxiv, 2021.02.24.21252329; doi: https://doi.org/10.1101/2021.02.24.21252329, https://www.medrxiv.org/content/10.1101/2021.02.24.21252329v1