Early in the pandemic of coronavirus infection (COVID-19) in the UK, it was believed that around 6% of the national population and 13% of the population of London were infected with severe coronavirus respiratory syndrome 2 (SARS -CoV-2). Most of the research and media response to the pandemic focused on the short-term effects and deaths, directly and indirectly, associated with COVID-19. However, more attention needs to be paid to the long-term effects of the disease to improve the capacity and delivery of health care.
Much academic and clinical work has focused on respiratory manifestations of SARS-CoV-2 disease, despite growing evidence for multi-organ and indirect effects on other organs and comorbidities. , such as cancers and cardiovascular diseases, as a result of lower healthcare access. The epidemiology of the so-called post-COVID syndrome (PCS) is not clearly defined. The available evidence reveals significant changes in estimates of PCS frequency and frequency as a result of changes in study numbers, sample sizes, recruitment methods, and follow-up times.
A retrospective study to determine organ loss levels after recovery from COVID-19
Recently medRxiv* introductory paper, researchers from the UK considered how they determined the levels of organ weakening after recovery from COVID-19-related hospitalization and compared the results with that in control group. They also examined how the rate ratio (RR) varies across gender, age, and ethnicity.
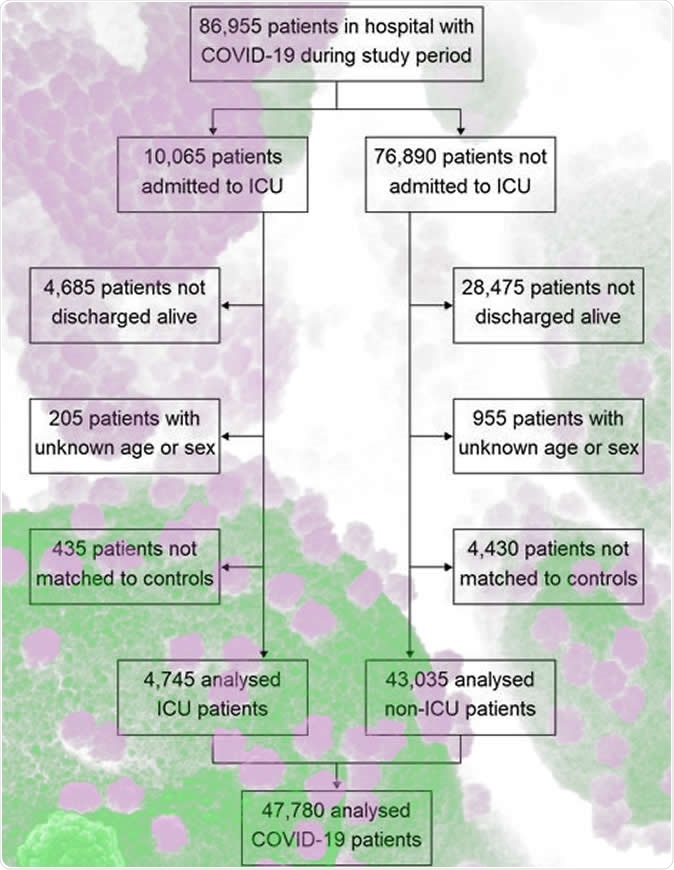
The observational, retrospective, similarity study was conducted in NHS hospitals in England. The study participants included 47,780 people with an average age of 65 who were hospitalized with COVID-19 and discharged by 31 August 2020. Approximately 55% of the study group were male, and the group was matched to controls on demographic characteristics as well as clinical characteristics. The main outcomes measured were multifactorial mortality rates, readmission to hospital, and diagnosis of cardiovascular, respiratory, metabolic, liver, and kidney diseases to 30 September 2020.
Examine a population flow diagram
People with PCS had higher rates of respiratory, cardiovascular and diabetes events
The average follow-up time for COVID-19 cases was 140 days, and the time for controls was 153 days. In COVID-19 cases, 766 (95% confidence interval: 753 to 779) and 320 (312 to 328) deaths were reported per 1,000 year-olds, i.e. 3.5 (3.4 to 3.6) and 7.7 (7.2 to 8.3) times greater, respectively, than in controls.
Levels of respiratory, cardiovascular, and diabetes events were also significantly increased in COVID-19 cases, with 770 (758 to 783), 126 (121 to 131), and 127 (122 to 132) events per 1,000 person year, individually.
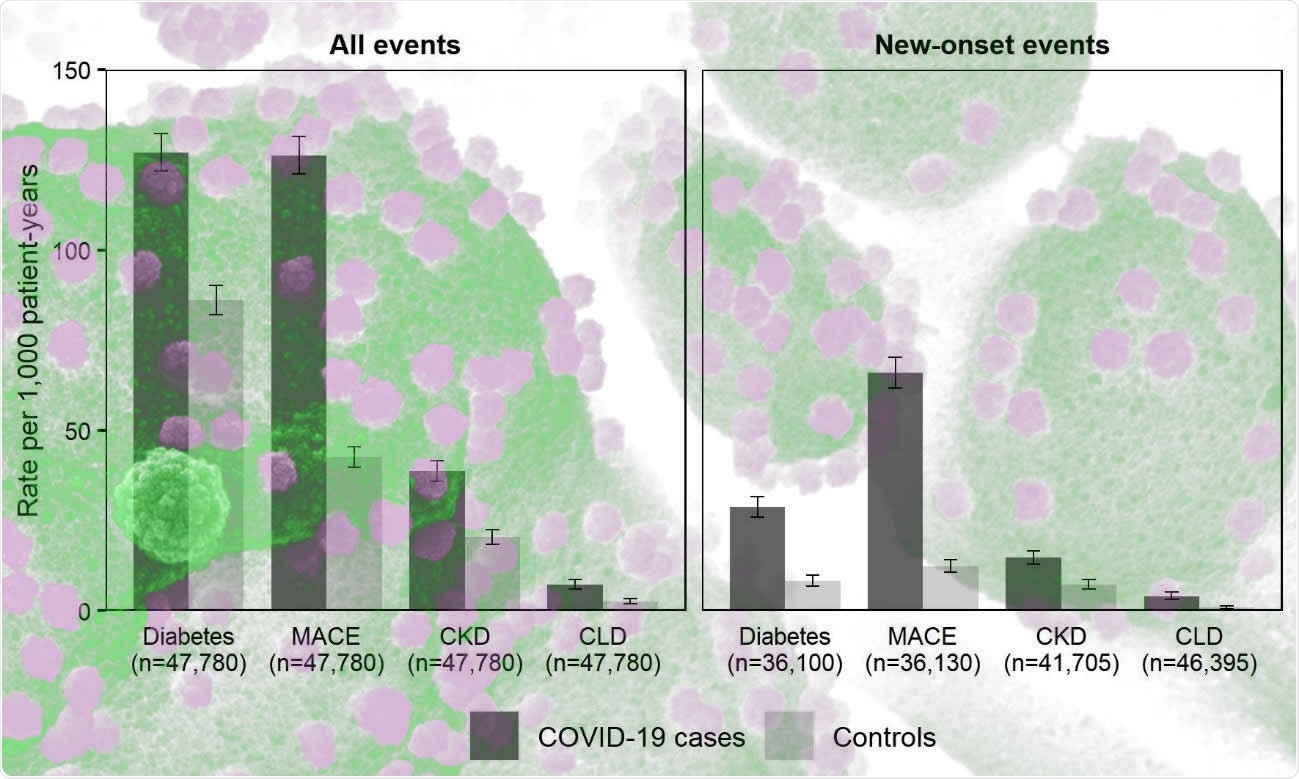
Incidence rates compared to COVID-19 individuals in England discharged from hospital by 31 August 2020 with similar controls
RR was higher for people younger than 70 compared to those aged 70 or older. RRs were also higher in minority ethnic groups compared to the White population. The most significant differences were found in respiratory disease: 10.5 [9.7 to 11.4] for persons under 70 years of age against 4.6 [4.3 to 4.8] for people aged 70 or over, and 11.4 (9.8 to 13.3) for a non-white population versus 5.2 (5.0 to 5.5) for the White population.
“Individuals discharged from hospital after a hungry COVID-19 face high rates of mortality, readmission, and multi-organ disorder compared to those of background levels are for these people, and the relative increase in risk is not limited to the elderly or clothing across ethnic groups. “
There was no increased risk for multiple organ disorders across different races
Based on the findings of the study, the authors concluded that people discharged from hospital after COVID-19 infection have higher rates of multi-organ disorder compared with control levels. . Interestingly, the increased risk was not limited to seniors or clothing across different races. Diagnosis, treatment, and prevention of long-term COVID-19 complications require integrated approaches rather than organ- or disease-specific approaches. According to the authors, more research is urgently needed to establish the risk factors for PCS.
“Integrated care pathways are structured, multidisciplinary care plans for specific diseases, which have been effective in other diseases such as obstructive pulmonary disease and may be useful in the management of PCS.”
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical / behavioral practice, or be treated as information established.