Present Mycoplasma salivarium in the lower airways of ventilated patients with COVID-19 infection it is associated with increased morbidity of mortality. The result was part of a molecular study that looked at how airway microenvironments affected severe respiratory syndrome (SARS-CoV-2).
Leopoldo N. Segal and colleagues suggest that lung microbes may be predictors of COVID infection and antibody resistance.
“These data highlight the importance of SARS-CoV-2 abundance in the lower airways as a predictor for mortality, and the significant contribution of host cell transcription, which is lower airway cell response to disease, “the researchers wrote.
The findings could help identify the patients most at risk for adverse clinical outcomes and provide other early treatments.
The study “microbial signatures in the lower airways of COVID19 patients with mechanical ventilation associated with poor clinical outcome” is available as a preview of the medRxiv* server, while the article is under peer review.
Classification of microbial signatures
The lowest air samples collected from patients ventilated from COVID-19 infection during the first wave in New York City. They collected airway samples from 142 patients with COVID-19 infection.
Mycoplasma salivarium in the airways associated with worse clinical outcomes
Using metagenomics, the researchers linked the microbes that resided in the lung midge with the clinical results of patients.
Results showed that there were many levels of Mycoplasma salivarium it was associated with a higher viral load of SARS-CoV-2. In addition, a limited immunoglobulin response in the lower airways was associated with an increased risk of death.
“The data presented here through the use of direct quantitative methods (RT-PCR) and an untested semicircular approach (metatranscriptome series) support the view that viral transport of SARS-CoV-2 in the lower airways in clinical progression of critically ill patients with COVID-19, “the researchers wrote.
There is no evidence of worse clinical outcomes from concussion with respiratory pathogens
While most patients received broad-spectrum antibiotics and antifungals, there was no evidence that side effects were exacerbated by coinfection with bacterial, viral, and fungal respiratory pathogens.
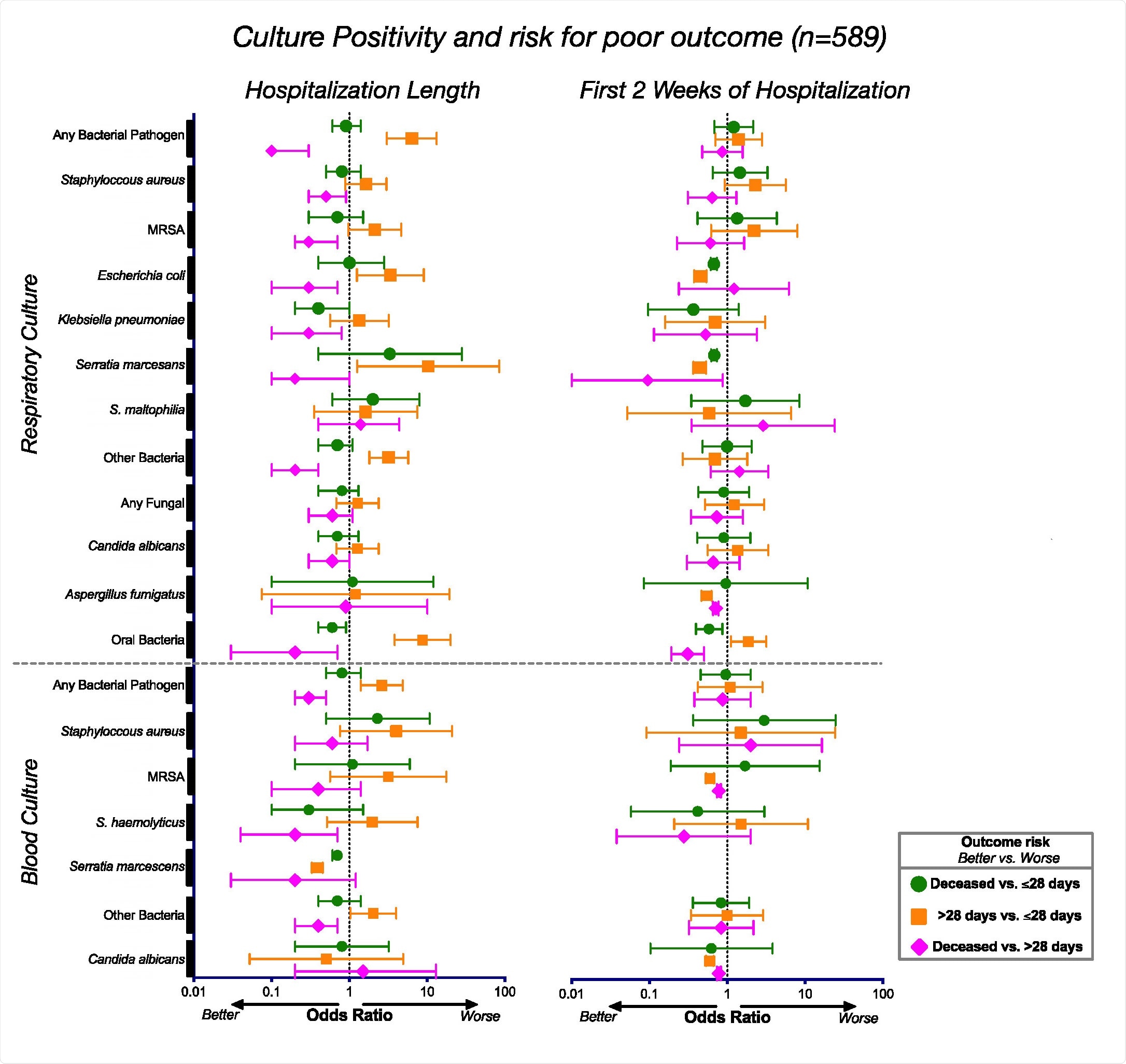
To look at the risk of mortality from COVID-19 infection, the team analyzed lab cultures from 589 hospitalized patients for respiratory failure from COVID-19 infection.
Results showed that patients with poor clinical outcomes did not respond to other respiratory diseases. There was also no association between advanced microbial cultures and mortality in severe COVID-19 diseases.
Links between cultural sensitivity and clinical outcome. Choice ratios and 95% confidence intervals correspond to culturally favorable levels for the whole group (n = 589) during the hospital stay (left) and during the first 2 weeks in the hospital (right).
Bacterial changes seen in patients ventilated for more than 28 days
Looking beyond microbes, the lower airways showed a high presence of SARS-CoV-2, which was associated with death. A tiny sample of patients had influenza A or B viruses, suggesting that the flu did not appear to have occurred at the same time as coronavirus infection.
When monitoring bacteria in the lower airways, metatranscriptome phages data actively detected the presence. The researchers suggest that this may be evidence that changes in the bacterial microbome may occur in patients with severe COVID-19 infection.
Changes were observed in Staphylococcus pagans, and Mycoplasma salivarium it was actively present in patients who required ventilation for more than 28 and patients who died compared with patients who were ventilated for less than 28 days.
Microbial effect on the immune response
Patients with poor clinical outcomes reported gene expression pathways associated with contamination, transport, as well as anti-microbial expression and symptom expression.
The researchers write:
“These differences may reflect important functional differences leading to a different metabolic environment in the lower airways that may affect host immune responses. It may also represent differences in microbial pressure in patients with higher viral loads and different inflammatory environments. “
There was also an increase in the Sirtuin and Ferroptosis signal pathways in the most severe COVID-19 cases. This coincided with inactive immune response features, including phagocytes, neutrophils, granulocytes, and leukocytes. Decreased immunoglobulin sensitivity levels and mitochondrial dysfunction were also observed.
Based on the data, the team recommends that the lungs of critically ill patients who need ventilation from COVID-19 infection report an unbalanced state rather than elevated inflammation. Doing this seems to predict the prognoses of worsening prognosis.
Further analysis of survival-related differences found in interferon responses. Activation of type I interferon was a predictive factor for increased mortality.
“While more long-term data will be needed to clarify the role of interferon markers on the disease, the data presented here suggest that a combination of names may be needed. microbial and host writing help to understand the increased risk for mortality in patients with severe COVID-19. “
*Important notice
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.