
Among the 2019 pandemic coronavirus infection (COVID-19), healthcare workers (HCWs) have been at work and are at risk of becoming infected with severe coronavirus respiratory syndrome (SARS- CoV-2), the causative pathogen of COVID-19.
A new study by U.S.-based researchers – at the Northwest Center for the Study, Education and Clinical of Mental Illness and Columbia University – has found that health care workers have experienced a lot of psychiatric anxiety during pandemic.
Pandemic and coronavirus
The coronavirus pandemic first appeared in Wuhan City, China, in December 2019. Since then, it has spread to 191 countries and regions, affecting more than 76.79 million and killing more than 1.69 million people.
Due to the scale and speed of the spread of the virus, health care systems in many countries were overrun, and there was a shortage of hospitals of intensive care unit (ICU) beds, personal protective equipment (PPE), and staff.
The impact of prolonged physical and emotional stress on HCW and first responders (FR) working through the pandemic has attracted much media attention. Previous studies have also addressed the physical and emotional pressures among these employees, linked to severe personal distress and reduced professional longevity.
Previous studies have linked the pandemic to higher mental health symptoms among health care workers, including depression, insomnia, anxiety, and post-traumatic stress disorder (PTSD).
A study in New York found increased use of medical leave, leading to a reduction in employee access among health care workers.
Great anxiety
The study, which appeared on the introduction medRxiv * server, aimed to determine the relationship between COVID-19 weight gain frequency and psychometric rating scale scores among HCW / FR. The team also wanted to find out if the psychosocial ranking scores affect job function and work longevity.
To reach the conclusions of the study, the team assessed the level of depression, insomnia, anxiety, and PTSD symptoms in both traditionally described HCW, as well as in FR, such as police officers, -fire, and EMTs working through the pandemic.
The study included 118 HCW and FR care for COVID-19 patients in the United States. The team used the PTSD checklist (PCL5), Patient Health Questionnaire (PHQ9) for depression, Insomnia Deficiency Index (ISI), and the generalized anxiety disorder 7 (GAD7).
The team has found that 31% of the 104 participants who completed a COVID-19 occupational exposure assessment had been diagnosed with known or similar COVID-19. Another 19% reported a close family member who had been ill with known or similar COVID-19, and 12% reported the death of a family member as a result of COVID-19. About 30% also reported having underlying health conditions that put them at increased risk of COVID-19.
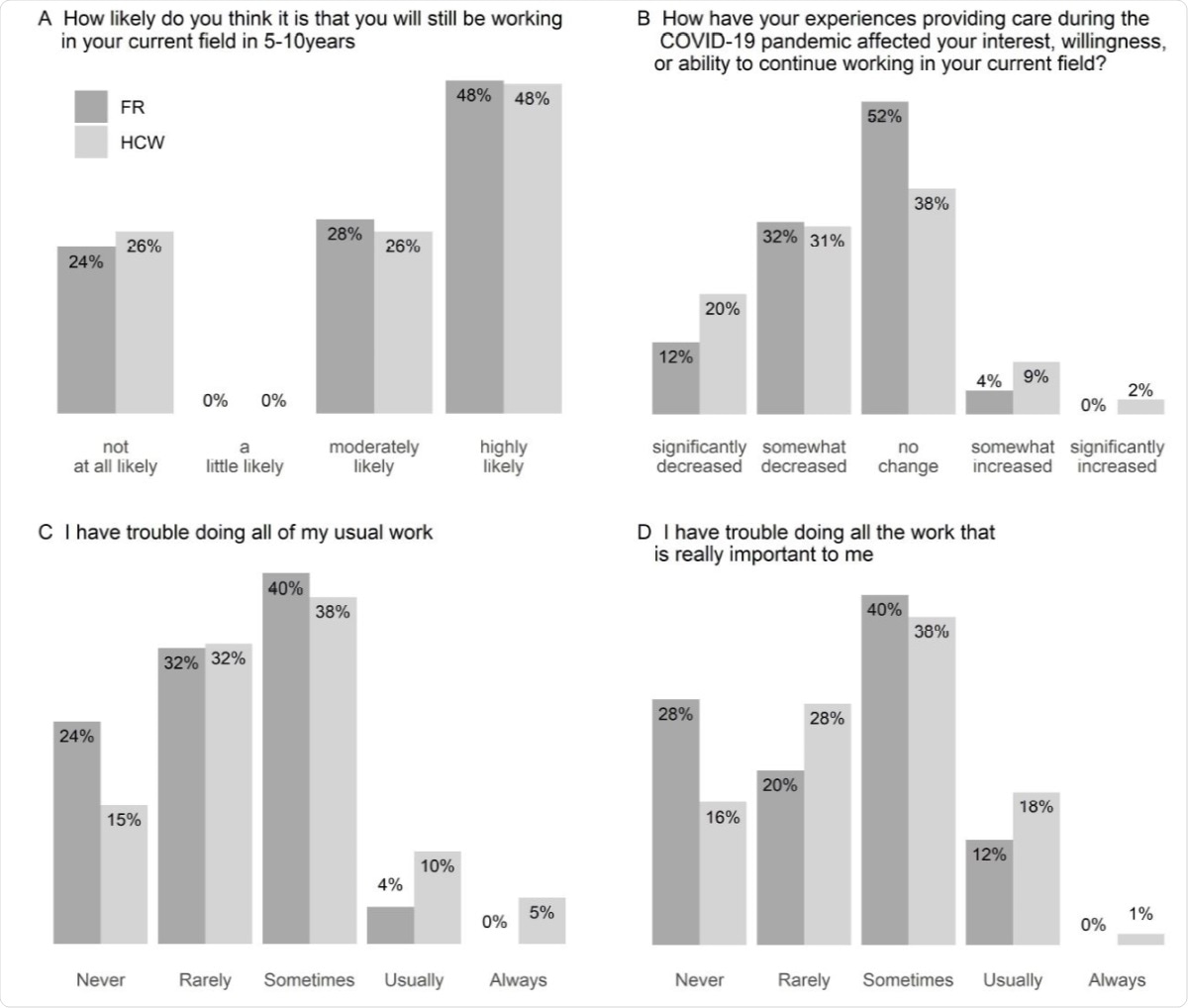
Dissemination of responses to self-report in maintenance and site work. Answers to questions about participants’ expectations of continuity in their current field (A, B) and current activity (C, D) for health care workers (HCW, n = 80) and first responders (FR, n = 25).
The team found that 26% of participants with an overall PCL5 score of 31 or higher, showed signs of PTSD. These are symptoms that are usually followed by traumatic stress. In terms of depressive symptoms, 60% of participants received an overall PHQ9 score above the normal threshold for mild depression, and 28% had an ISI score for lower moderate insomnia. Finally, 67% received a GAD7 score for moderate anxiety.
These results focus directly on the identification of potentially treatable psychiatric symptoms, particularly those at PTSD, in HCW and FR suffering from COVID-related stressors. 19, “the researchers concluded.
The findings of the study showed that HCW / FR experiences during the pandemic had an impact on their interest, willingness or ability to continue working in their current field.
Many of the two organizations stated that their experience of working at the Covid-19 pandemic was likely to remain in their current range of experience. , and at least sometimes have difficulty completing their normal or important work, “the researchers added.
The researchers recommend COVID-19-related weight loss among HCWs and FRs whenever possible, such as by providing appropriate PPE and other measures. These can help improve their mental health, work function, and retention in the health care workforce.
* Important message
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or treated as fixed information.
Source:
Magazine Reference:
- Hendrickson, R., Slevin, R., Chang, B., Sano, CE, McCall, C., and Raskind, M. (2020). The impact of working at Covid-19 pandemic disease on health care workers and first responders: mental health, functioning, and professional retention. medRxiv. doi: https://doi.org/10.1101/2020.12.16.20248325,https://www.medrxiv.org/content/10.1101/2020.12.16.20248325v1