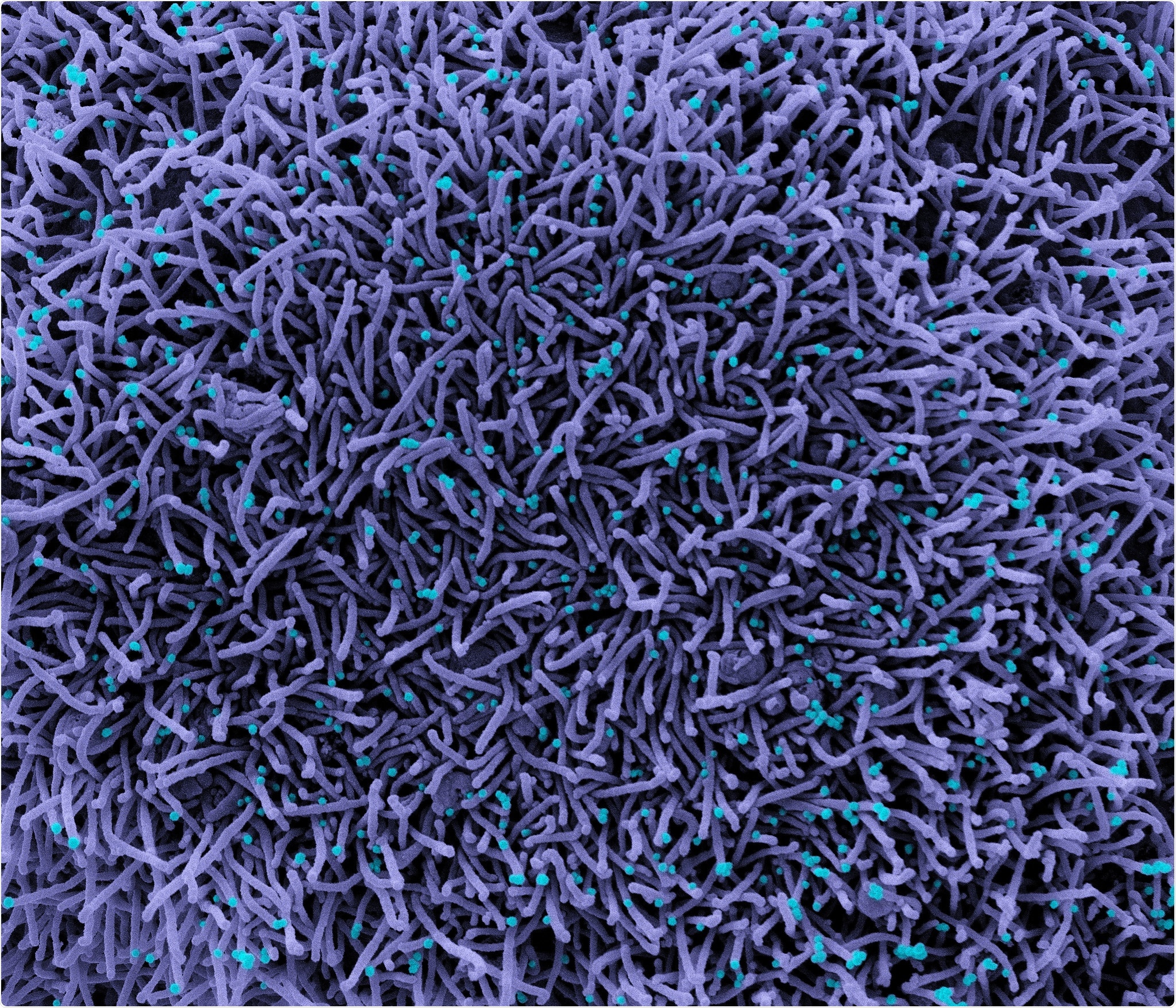
Researchers in the United States and Canada have mapped the presence of acute coronavirus respiratory syndrome 2 (SARS-CoV-2) in the brains of people who died from coronavirus disease 2019 (COVID-19).
Geidy Serrano of the Banner Sun Health Research Institute in Sun City, Arizona and colleagues found that infection with SARS-CoV-2 can lead to starvation neuropathology.
The findings supported other studies suggesting that neurological signs and symptoms are not usually the result of a direct viral attack on the brain. Instead, they appear to be associated with systemic reactions such as coagulopathy, autoimmune responses, organ failure and sepsis.
The team says much remains to be understood, including the interaction between viruses and hosts that affect brain attack and whether the virus is cleared from the brain after a serious illness.
A pre-printed version of the research paper can be found on the medRxiv* server, while the article is subject to peer review.
SARS-CoV-2 is associated with other invasive brain coronaviruses
Because the SARS-CoV-2 virus is associated with previously shown coronaviruses attacking the brain, SARS-CoV-2 appears to share similar capabilities, say the research.
The human coronavirus OC43 (HCoV-OC43) has been found to cause acute encephalomyelitis in children, while other coronaviruses have been linked to demyelinating disease in animal studies.
The HCoV-OC43 virus and another strain – HCoV-229E – have also been found in human brains acquired from many banks across Europe, the UK and the United States, suggesting that coronaviruses have the ability to attack take it on and keep going in the central nervous system (CNS).
Numerous clinical reports and reviews have collectively described a wide range of signs, symptoms, and syndromes associated with SARS-CoV-2. However, it is not clear what fraction of the result has been a direct viral CNS attack compared to indirect effects caused by systematic reactions to acute illness.
Autopsy reports have described meningitis and encephalitis in a small fraction of patients dying from COVID-19 and, more frequently, ischemic and hemorrhagic cerebrovascular injuries. However, these findings are not supported by direct evidence of SARS-CoV-2 in the CNS.
“Critical deficits are still a complete clinical-based study of the presence of CNS or specific neuropathology of SARS-CoV-2 in humans,” says Serrano and colleagues.
What did the researchers do?
Using reverse chain transcriptase-polymerase (RT-PCR) assays, the researchers conducted a comprehensive study of the presence of SARS-CoV-2 RNA in 16 brain regions of 20 people who had died from COVID-19.
The subjects ranged in age from 38 to 97 years (average age 77 years), and 11 were male.
The majority of those who died from COVID-19 exhibited normal age-related neuropathologic features.
Only two individuals had severe neuropathology, one with severe cerebral obstruction and one with hemorrhagic encephalitis. In all cases, the neuropathology was inextricably linked to COVID-19.
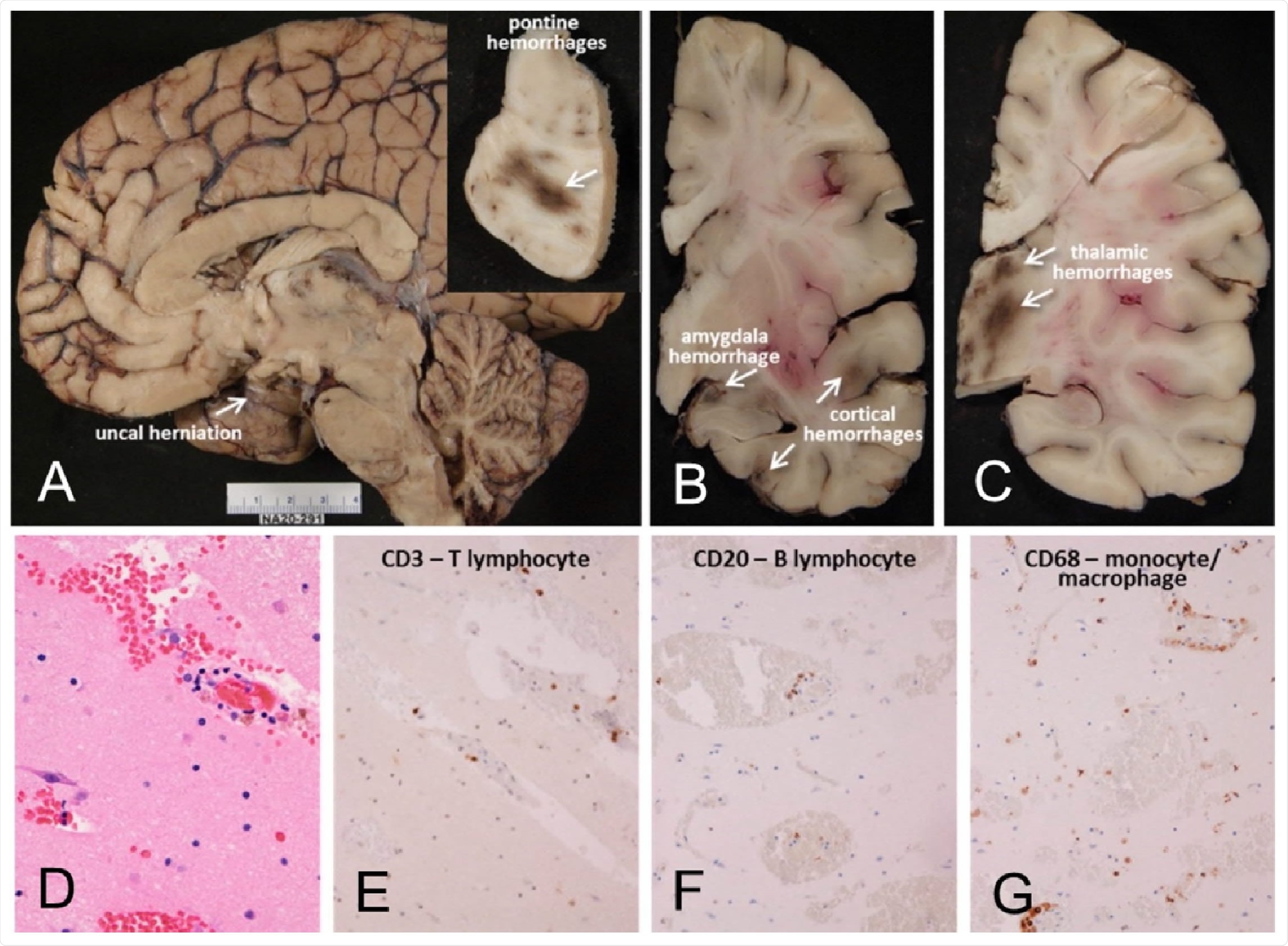
The case of the Mayo M10 Clinic, a man in his 30s. Full neuropathological examination consistent with brain inflammation associated with encephalitis causing transtentorial (A) uncallern herniation and associated with acute hemorrhages (inset A arrows, and in B and C). Microscopic examination of semiadjacent temporal lobe sections reveals microscopic hemorrhage (stain D; H&E) and infiltration of neuropil w and B-lymphocytes and macrophages (EG)
However, most of the remaining subjects had nonspecific histopathology. Apart from the case of encephalitis and one case where two microglial nodules were observed in the posterior medulla, there was no clear evidence of classical neuropathology of CNS viral diseases.
“The findings of this study are generally in agreement with previously reported autopsy studies on the brains of COVID-19 disease subjects, as severe complications such as encephalitis and severe hunger infarctions were present in very few subjects,” he said. the team.
Has SARS-CoV-2 RNA been detected?
The study identified four individuals (20%) who had SARS-CoV-2 RNA in one or more brain regions, including the olfactory bulb, amygdala, entorhinal region, temporal and frontal neocortex, dorsal medulla and leptomeninges .
The team says the relatively low level of SARS-CoV-2 RNA in brain tension also agrees with previous studies. The 20% rate observed here compares with an average of 22% over the total number of people included in 16 previously published studies.
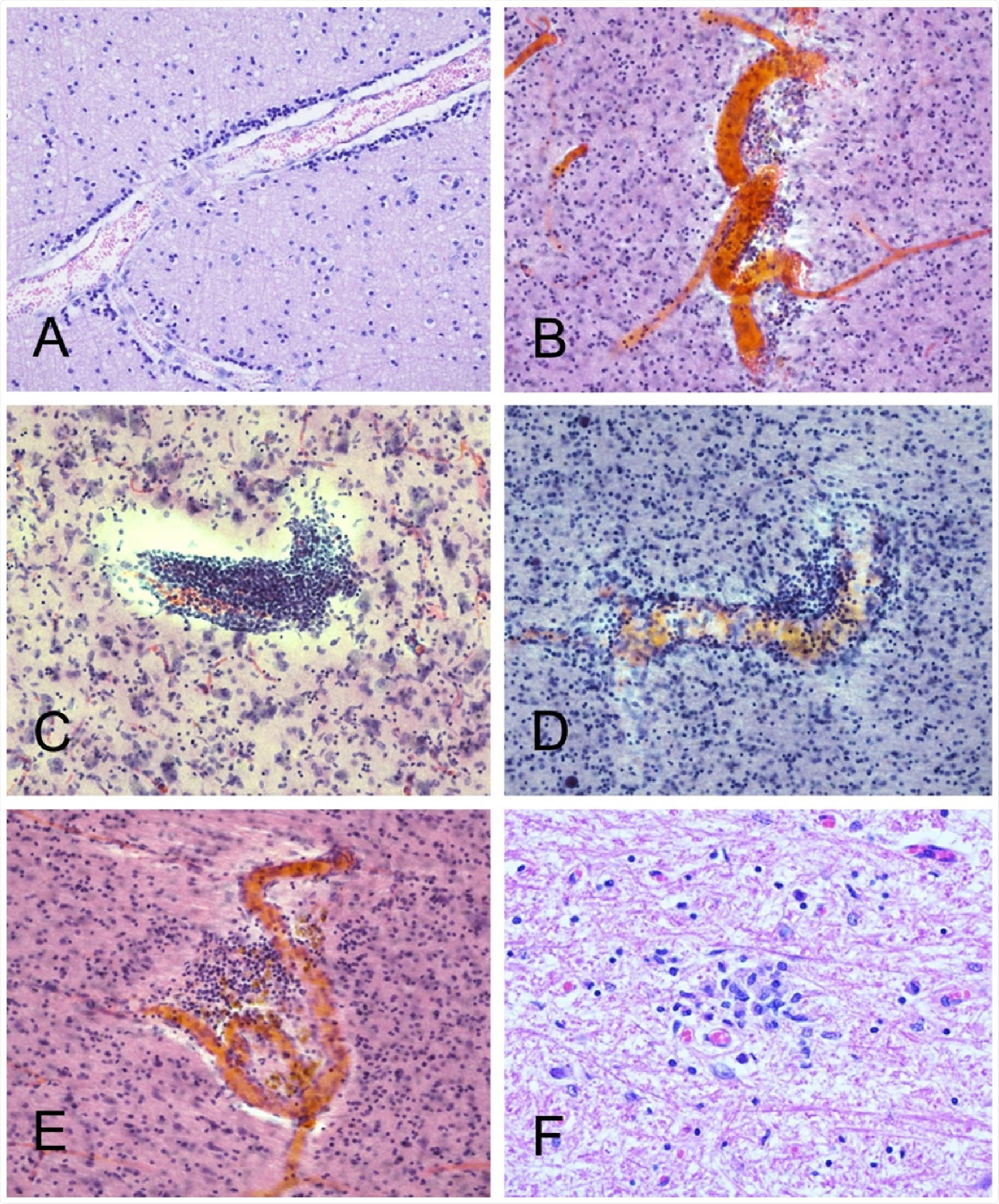
In several cases there were perivascular mononuclear cell accumulations, both gray and white. Examples can be seen from BSHRI Case B4, male in his 80s (A), Case B2, woman in her 70s Case B6, male in his 70s (C), Case B8, male in his 80s (D), and Case B9, a man in his 70s (E). There is also a microglial nodule in the posterior medulla in the area of the nucleus gracilis, in BSHRI Case B6 (F) Images are from H & E-stained sections 80 μm thick (BE) or 6 μm paraffin sections (A, F).
What is the impact of the study?
“These results confirm the growing consensus that most of the associated neurological signs and symptoms associated with COVID-19 may be the result, not the viral brain attack, but to systematic reactions such as coagulopathy, sepsis, autoimmune mechanisms or multiorgan failure, ”the team wrote.
The researchers say that, like other human coronaviruses, SARS-CoV-2 can lead to acute or subacute neuropathology.
However, much remains to be understood, including the host-virus interactions that affect CNS attack and whether the virus is cleared up after a serious illness.
“We hope that further studies will allow the development of better diagnostic, diagnostic and treatment strategies,” Serrano and colleagues concluded.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.