Since the outbreak of coronavirus pandemic 2019 (COVID-19), caused by the severe respiratory coronavirus 2 (SARS-CoV-2) syndrome, millions of people have died, with more than one hundred million infections reported worldwide the world. Some groups are particularly vulnerable to the virus, developing a progressive disease.
The World Health Organization has identified pregnancy as a high-risk group for COVID-19, especially in pre-existing medical conditions, advanced maternal age, and high body mass index (BMI). The main adverse outcomes include more severe infection and premature birth.
Population-based studies are essential to gain knowledge of the spread and management of this disease. However, most studies of pregnancy during COVID-19 had not been as generally relevant to Scandinavian populations, as the majority of routine COVID-19 studies in general.
A new study, featuring the introduction medRxiv * server, aiming for pregnancy in those countries only to get decisions on the connection of these conditions.
In Scandinavian countries, the population mix is far more uniform than in most developed countries, while health care in pregnancy is free. All pregnancies and their outcomes are recorded in medical birth records. This well-cared for single-sex fertile group is therefore assessed separately in the current population-based study.
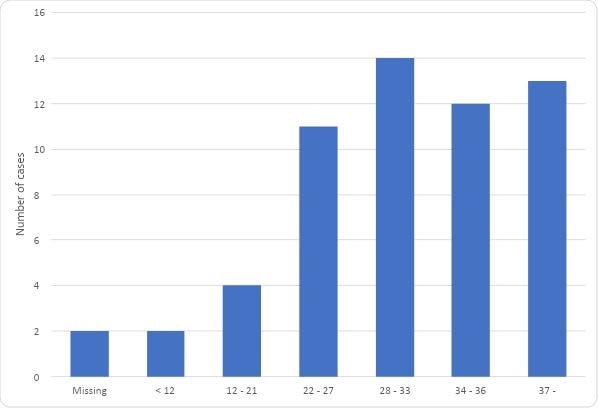
Gestational week completed at first SARS-CoV-2 positive PCR test in 56 pregnant women admitted to hospital for COVID-19 in the Scandinavian countries between 1 March and 30 June 2020
Risk features and factors
From March to June 2020 (both months inclusive), 214 admissions of pregnant women were diagnosed with COVID-19. The diagnosis was based on a positive RT-PCR (reverse transcriptase-polymerase chain reaction) response within 14 days of its introduction. The entry rate varied widely, from less than 1 per 1,000 deliveries in most Scandinavian countries to above 18 per 1,000 in Sweden.
Since not all of these admissions were due to COVID-19 per se, the remaining analyzes were performed on a subset of 56 pregnant women who required admission only because of COVID- 19.
The three Swedish hospitals in this study account for about one-fifth of the total number of births in this country, which allows for a large under-reporting of COVID-19-related admissions and outcomes. In addition, the reported cases from these university hospitals may suffer from selection bias.
In this group, hospital admission rates ranged from 0.3 to 0.5 per 1,000 deliveries in most Scandinavian countries to nearly 4 per 1,000 in Sweden. No hospitalized cases of pregnancy due to COVID-19 were reported from Iceland over the first four months of the pandemic.
The majority of women admitted because of the disease were in pregnancy in their third trimester when they were diagnosed. Most were obese with a BMI above 30, and most were migrants.
In Sweden, more women admitted to COVID-19 had other co-infections than in other Scandinavian countries.
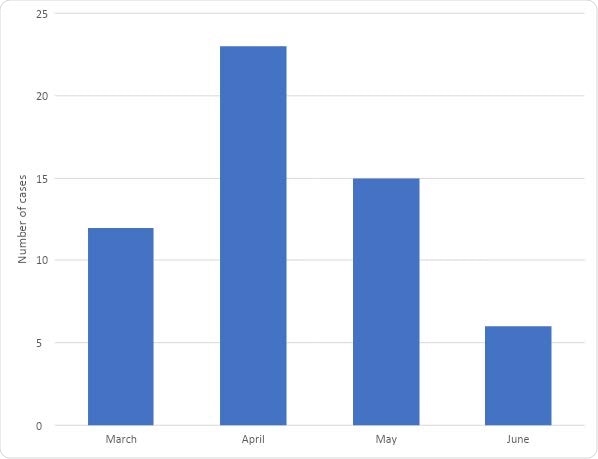
One month of the first advanced SARS-CoV-2 PCR test in 56 pregnant women admitted to hospital for COVID-19 in Scandinavia, 1 March and 30 June 2020
Again, of the nearly 30% of those women who had multiple pregnancies, 90% were in Sweden. Finally, Swedish women tended to undergo a positive test at later terms and delivered earlier after diagnosis.
Swedish cases came from tertiary care hospitals, which may be due to the higher number of multiple body movements complicated by multiple births and underlying conditions in this country. The use of universal obstetric screening in one of the three Swedish hospitals included in this study may explain the lower levels of preterm and cesarean delivery, as it does not. cases from the other countries included only very poor COVID-19 demonstrations during pregnancy.
Management and outcomes of COVID-19 in pregnancy
Of the 56 pregnant women hospitalized with COVID-19, 12 women required admission to an intensive care unit (ICU). None of the women died from COVID-19.
Labor entry was slightly more common in Sweden than in other countries, but Cesarean delivery rates were lower, at ~39% vs. 53%, respectively.
49 babies were born to 48 women during this period, and ~ 42% were delivered by Cesarean. This is a larger proportion compared to 1717% in 2018. Emergency Cesarean rates were also higher, at 85% vs. 54%, compared to 2018 levels.
Women with COVID-19 had higher rates of preterm delivery in pregnancy, at 25% vs. ~ 6% in 2018.
Seven of the infants required admission to the Neonatal ICU (NICU), but no fatalities or infant deaths were reported. NICU admissions were lower in Sweden, at 77%, compared to 2828% in other Scandinavian countries.
What is the impact?
This prospective study covers only pregnant women with the most severe forms of COVID-19, thus eliminating bias due to different testing strategies in different countries. The results show that hospital risk in pregnancy due to COVID-19 is low, and the outcome generally favorable.
Perhaps the fact is that more than a fifth of the women needed to be admitted to ICU because this study only covered the most severe cases. Earlier studies have shown that pregnancy increases the risk of ICU admission for COVID-19.
Interestingly, admission rates were higher in Sweden than in other Scandinavian countries, possibly reflecting the higher rates of hospitalization and ICU admission in the general population. in the previous region.
“This may indicate that policies that reduce transmission in the general population also reduce hospital admissions due to COVID-19 among pregnant women. with a child. ”
Obesity and a non-Scandinavian origin tended to increase the risk of hospitalization. This experience has the potential to shape public health policies aimed at reducing the risk of adverse outcomes in this group.
Women admitted to pregnancy as a result of COVID-19 were more likely to deliver preterm or by cesarean section, in agreement with other studies showing that these results are increasing by the severity of COVID-19.
Risks associated with pregnancy of adverse outcomes due to COVID-19 depend on national public health strategies and the spread of the virus at a population level. International collaborative studies help evaluate less common complications and risk factors that may affect obstetric outcomes during the pandemic.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.