In December 2019, a ‘major viral infection of unknown cause’ was identified in Wuhan, China, which was later identified as the most severe respiratory respiratory coronavirus 2 (SARS-CoV-2) syndrome.
SARS-CoV-2 infection causes COVID-19 (coronavirus disease 2019) and is characterized primarily by cough, fever, fatigue, and high respiratory distress syndrome (ARDS) associated with high mortality rates.
On March 11, 2020, the World Health Organization (WHO) officially declared the coronavirus revolution as a pandemic. To date, SARS-CoV-2 infection has diagnosed more than 106 million cases. According to the WHO, it has killed more than 2.3 million.
Writing in the International Journal of Nanomedicine, Professor Dongki Yang, from the Department of Psychology, Gachon University, South Korea, has reviewed the available knowledge about the coronaviruses, routine approaches to dealing with their newly emerged SARS-CoV-2 infection, and innovative use of nanotechnology in the COVID- 19 pandemic.
Corona-viruses
Coronaviruses (CoVs) are RNA viruses, 27–32 kb (kilobases) in size, and belong to the Coronaviridae family. These viruses affect humans and other animals. These rapidly growing human coronaviruses (due to their high nucleotide genomic reabsorption rates) cause bronchiolitis, pneumonia, and also the common cold.
There are currently seven known human coronaviruses: (HCoV-229E, HCoV-NL63, HCoV-HKU1, HCoV-OC43, Middle East respiratory syndrome coronavirus (MERS-CoV), SARS-CoV, and SARS-CoV-2).
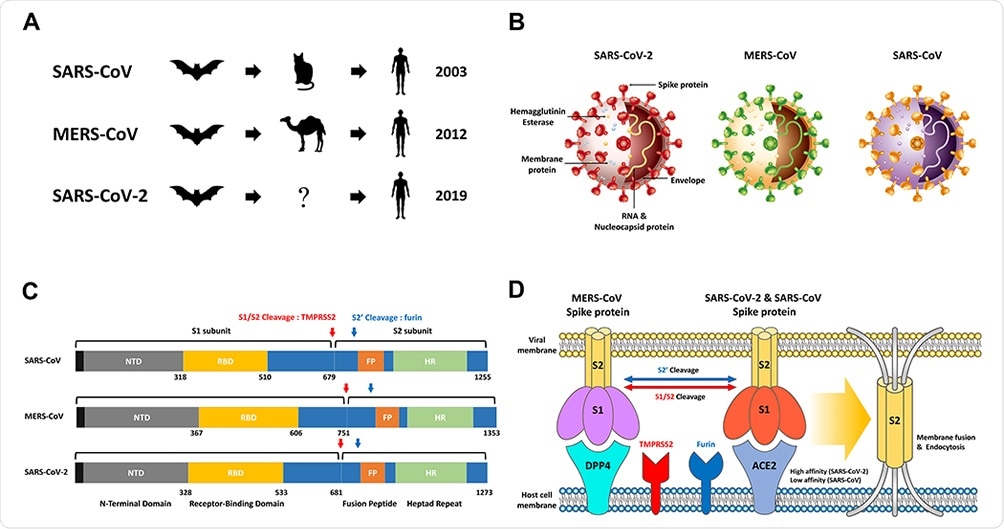
Overview SARS-CoV, MERS-CoV, SARS-CoV-2. (A) The origins of SARS-CoV, MERS-CoV and SARS-CoV-2 are widely recognized as bats as native hosts. While SARS-CoV and MERS-CoV have been shown to be intermediate hosts in civets and camels, SARS-CoV-2 can introduce humans through an intermediate host that is not yet known. Following animal disease, SARS – CoV – 2 has so far spread rapidly worldwide, mainly through continuous human – to – human transmission. (B) Concentrated structure of SARS-CoV-2, MERS-CoV and SARS-CoV including Hemagglutinin Esterase, membrane protein, RNA & Nucleocapsid protein, Envelope, and Spike protein. (C) Comparison of the S proteins of SARS-CoV, MERS-CoV and SARS-CoV-2. NTD, RBD, FP, HR, and Cleavage sites with TMPRSS2 and furin. (D) The proteins MERS-CoV, SARS-CoV, and SARS-CoV-2 S bind to ACE2 and DPP4, which are receptors present in host cells. In order for the S2 domain in the virus to dissolve to the host cell membrane to cause endocytosis, the cutting process at two sites (S1 / S2 and S2 ‘) through the Furin and TMPRSS2 proteases is critical. SARS-CoV-2 has a much higher affinity than SARS-CoV S and ACE2-binding proteins, resulting in a high disease rate.
These human coronaviruses are one of the 10 most well-known viruses that are deadly to humans. SARS-CoV mortality rate is up to 10%, and MERS-CoV mortality rate is 36%.
The structural and functional epidemiology of the SARS-CoV, MERS-CoV, and SARS-COV-2 viruses are described in the review, followed by therapeutic strategies.
Because of the most common mild-to-gen symptoms in the case of SARS-CoV-2, the asymptomatic spread of the virus has contributed to the rapid and widespread spread of the virus. Therefore, vaccines are essential.
At an unprecedented pace, vaccines were developed; similarly, scientists have also devised a combination therapy to fight this disease.
In this regard, nanotechnology offers many opportunities to fight the virus: nano-based formulas, nano-vaccine metastasis platforms, and nano-drugs.
Therapeutic Strategies
Several antiviral drugs approved for other applications have effects on SARS-CoV-2, but the results were different in small randomized trials. These include remdesivir, which was developed as an experimental drug against the Ebola virus (EBOV) during Ebola infection in West Africa, chloroquine (CQ) and hydroxychloroquine (HCQ) for malaria, and lopinavir / ritonavir (LPV / r). , which is used to treat acquired immunodeficiency syndrome (AIDS).
The spike protein interaction agents (S) and ACE2 (Angiotensin-Converting Enzyme 2) and the neutralizing antibodies inhibit virus transmission and immediate protection.
In immunotherapy, Tocilizumab (monoclonal antibody against IL-6) blocks the transmission of the signals that stimulate the inflammatory responses; IL-6 is one of the leading causes of inflammation, leading to severe consequences in COVID-19 disease. However, the costs and safety precautions may preclude the use of Tocilizumab in the treatment of COVID-19, the author wrote.
Many clinical trials are testing the convalescent plasma (CP) therapy, another effective method for the treatment of COVID-19 worldwide.
RNAi (RNAi) intervention is also a new therapeutic strategy for SARS-CoV because it can detoxify specific mRNAs.
Vaccine prevention strategies
Data from vaccine development for SARS-CoV and MERS-CoV contributed to the development of vaccine candidates for SARS-CoV-2. In unparalleled performance in vaccine development history, inactivated or live vaccines and reconstituted vaccines have been developed with high neutralization potential. Effective vaccines against the SARS-CoV-2 strains are now being given worldwide – starting the fight to eradicate the pandemic virus.
Application of nanotechnology in COVID-19 therapeutic therapy
Nanoparticles and viruses are comparable in size and function. Various treatments using nanotechnology have been developed and commercialized for common viral infections, such as IAV and IBV (influenza virus), EBOV (Ebola), HIV1 and 2 (human immunodeficiency viruses), HSV1 and 2 (herpes simplex virus), HBV and HCV (hepatitis B and C), and HuNoV.1 (human noroviruses).
“The accumulated advances in these virus-fighting nanotechnologies can play an important role in taking SARS-CoV-2 treatment and vaccine development to the next level. ”
Nanomedicines are emerging as effective alternatives to vaccine technologies. While vaccines are currently being delivered to humans, nanotechnology and nanomedicine are presented in the review as new therapeutic technologies and approaches that may soon have clinical implications.
Professor Dongki Yang talks on theranostic nanoparticles, nanoparticles delivery therapy, nanotechnology-based diagnostics, nanotechnology-based vaccine underdevelopment vaccines, other vaccines (nuclear acid vaccines and NP-based vaccines) ) and inactivation of SARS-CoV-2 in the outdoor environment using nanotechnology. .
Dexamethasones, the therapeutic agent of COVID-19 introduced through various nano-formulas, have led to a major reversal in the treatment of COVID-19.
Also, the Pfizer liposomal mRNA vaccine (BNT162b) is a high performance of nanomedicine, in which lipid-nanoparticle-modified mRNA (LNP) encoding is modified by SAS-CoV-2 glycoprotein spike.
Also, technologies that use nanomaterials, such as silver nanoparticles, copper or copper oxide nanoparticles, and gold nanoparticles, prevent and control COVID-19 by disabling the SARS-CoV- 2 in the environment. In the short term, nanotechnology and nanomedicine may be suitable options for this change in the research and development pattern, Dr. Yang suggests.