.jpg)
Researchers at GlaxoSmithKline (GSK) in Italy and Belgium say that the 2019 coronavirus pandemic (COVID-19) is changing the world of vaccination by accelerating vaccine development and the availability of powerful technologies.
The team says the pandemic has driven the development of technologies such as synthetic RNA vaccines and viral vectors by at least a decade.
Rino Rappuoli and his colleagues hope that these accelerated developments, together with advances in the field of immunotherapy, could help address some of the challenges facing the post-COVID world, such as emerging pathogens, resistance to chemicals, harmful diseases, and cancer.
“For example, RNA vaccines and viral vectors could be designed to encode not only antigens but also molecules capable of reactivating the immune system,” they write. .
Technological advances that have come together to develop the COVID-19 vaccine
COVID-19 paints a grim picture of a vaccine – free world
The COVID-19 pandemic has painted a worrying picture of the future without vaccines.
“Fortunately, new technologies, speed of understanding of new and existing pathogens, and greater knowledge of the immune system allow us today to develop vaccines at an unprecedented pace,” said Rappuoli and the team.
In a scene published in the Proceedings of the National Academy of Sciences, the researchers discuss the progress made in genome-based vaccine development and some of the challenges ahead where such vaccines could play an important role.
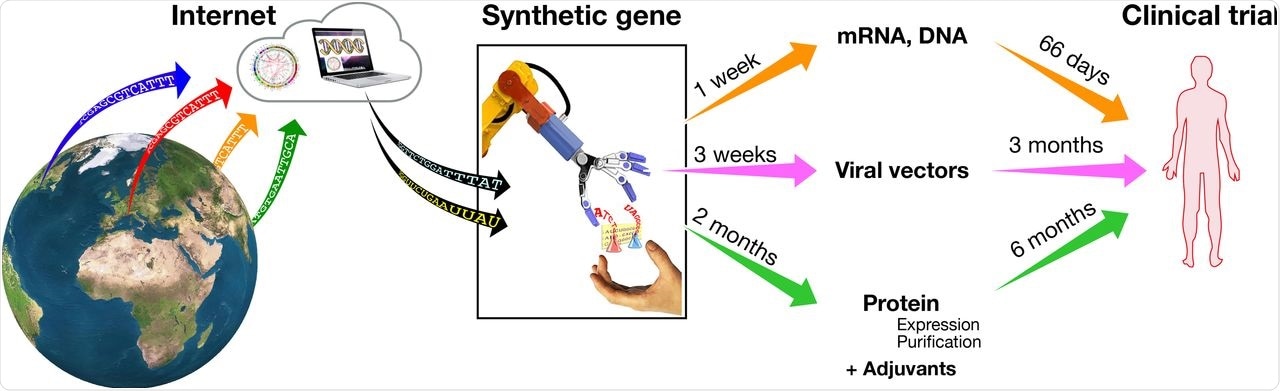
COVID-19 vaccines in development and their timeline to clinical trials in humans
Progress with genome-based vaccines began in 2013
Progress was first made with synthetic, genome – based vaccines in 2013 when researchers developed an RNA vaccine against an emerging and potentially contagious H7N9 flu virus.
For the first time, a fully synthetic viral vaccine was administered in vitro without cultivation of the virus. Instead, the genome sequence available in public databases available on the Internet was used.
The “internet-based vaccines,” developed using shared genomic information, avoid the need to carry, infect and grow the native virus.
“Fortunately, the H7N9 flu virus has not spread effectively between humans, and, although it has caused a few hundred cases in the next few years, it has not caused a pandemic, limiting the use of these vaccines to clinical trials only, ”wrote Rappuoli and colleagues.
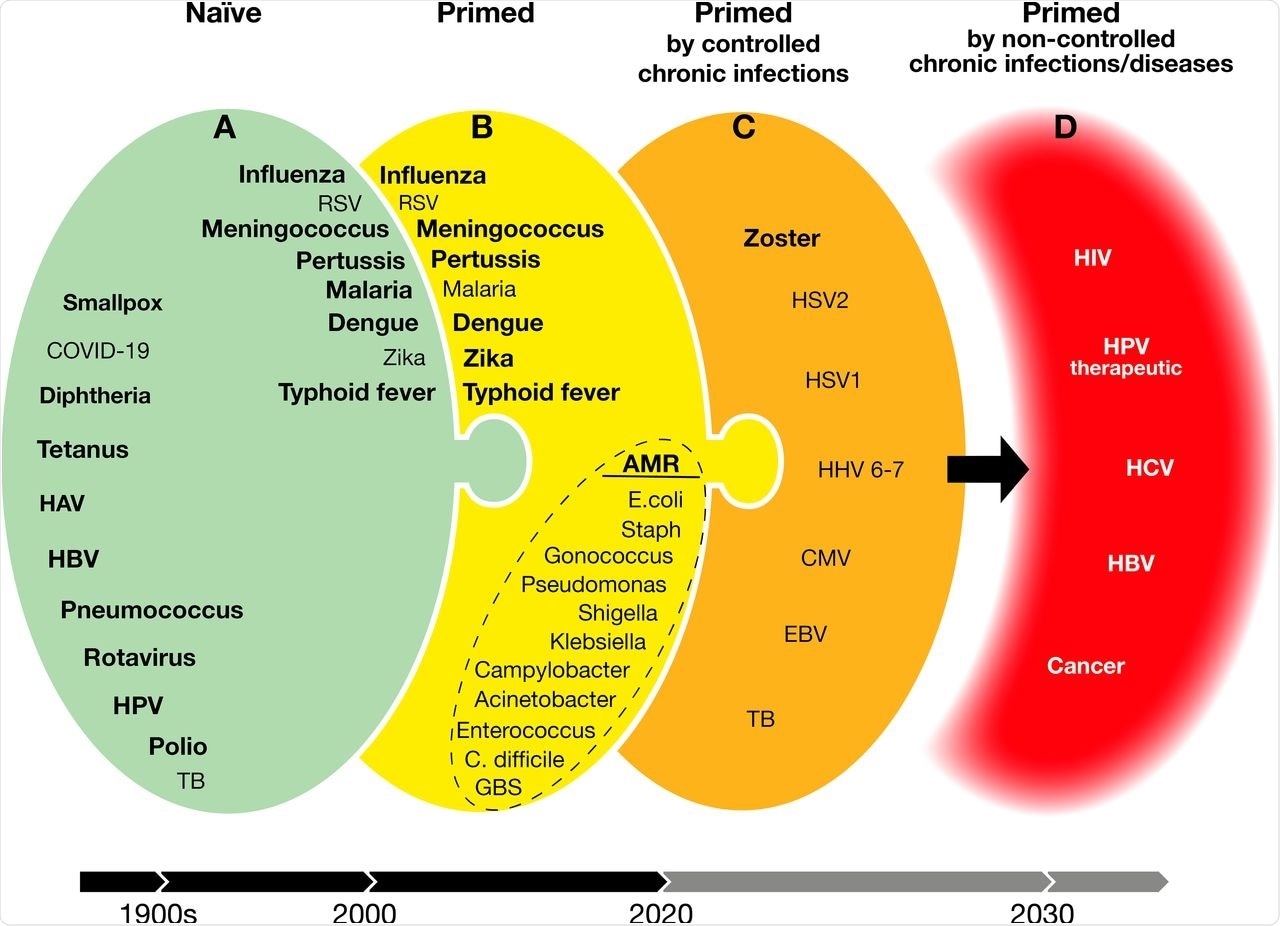
Develop vaccines to treat naïve, previously exposed, diseases and breast diseases. Green (A) vaccine is available or can be made with the latest technologies. Heavy vaccines, available. Yellow (B) and orange (C) are doable vaccines with growing challenges for today’s technologies. Red (D) are targets that we do not yet have the scientific knowledge and technologies. HAV, hepatitis A virus; HBV, hepatitis B virus; HPV, human papillomavirus; TB, tuberculosis; RSV, respiratory syncytial virus; AMR, chemical resistance; E. coli, Escherichia coli; Staph, Staphylococcus aureus; C. difficile, Clostridium difficile; GBS, group B Streptococcus; HSV1, herpes simplex virus 1; HSV2, herpes simplex virus 2; HHV, 6-7 human herpes viruses 6 and 7; CMV, cytomegalovirus; EBV, Epstein-Barr virus; HIV, human immunodeficiency virus; HCV, hepatitis C virus.
Labs around the world had the ability to make genomic vaccines prior to COVID-19
By the time the genomic sequence for acute respiratory respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent responsible for COVID-19 – became publicly available on the internet in January 2020, its most laboratories around the world are already able to make vaccines from synthetic genes.
Several methods are used to make COVID-19 vaccines, but here, the researchers focus on three main types of internet-based vaccines that are experiencing significant development acceleration: synthetic RNA vaccines , viral vectors, and protein-based vaccines.
Synthetic RNA vaccines are the fastest of the three to be developed. A fully synthetic gene, locked in a plasmid vector, serves as a template for in vitro synthesis of the RNA vaccine.
For viral vectors, there is a synthetic gene that encodes the viral spike protein that SARS-CoV-2 uses to enter cells into a virus that has been engineered to prevent reproducibility in humans. After being grown in culture, the virus is introduced into the body through a vaccine, delivering the synthetic gene to cells.
In the case of protein – based vaccines, a synthetic gene that encodes the spike protein or its receptor binding domain is used to engineer the mammalian, viral or plant – producing enzymes of the protein. This recycled protein is then purified and mixed with an adjuvant to form a vaccine.
Challenges facing the post-COVID world
The researchers say that the accelerated development of these RNAs and viral vectors has meant that these platforms are now available not only for emerging diseases but also for other imminent public health threats to the post-COVID world.
For example, antibiotic-resistant bacteria pose a significant risk to public health, with people potentially at risk of recurrent infection with pathogens such as Escherichia coli, Staphylococcus aureus, Clostridium difficile, Klebsiella pneumoniae, and Pseudomonas aeruginosa.
This chemical resistance (AMR) is effectively a growing pandemic that is expected to have a devastating impact on public health and the global economy over the next two years. decade, said Rappuoli and team.
However, vaccines can help tackle AMR, they say: “We have enough technologies and empirical knowledge to develop new vaccines for AMR.”
Chronic disease and cancer
In some cases, the immune system is completely overwhelmed by pathogens such as HIV or conditions such as cancer and the body is left vulnerable to chronic diseases. The immune system is unable to control the pathogen or cancer cells, which are then free to reproduce forever.
“Until now, we have not been able to make successful vaccines against these diseases, and we do not have the scientific knowledge to make them,” said the researchers.
However, immunotherapy studies have shown that, in the case of cancer, the lost immune system is characterized by regulatory T cells that are able to be activated using specific antibodies.
“The success of immunotherapy in the field of cancer and a greater understanding of the mechanical properties of the suppressed immune system suggest that vaccination may, in the near future, have an impact on breast cancer and diseases,” wrote Rappuoli and his co. -workers.
“It is possible that the rapid evolution of the newly discovered technologies for COVID-19 (RNA vaccines, viral vectors, and protein-based vaccines with strong confession) along with the learning will come from immunotherapy in response for some of the new challenges. of today’s society such as emerging diseases, AMR, breast diseases and cancer, ”the team concludes.