A team of scientists from the United States has recently studied the use of pericyte-like brain cortical organoids as an experimental model to study the effects of severe respiratory disease coronavirus syndrome 2 (SARS-CoV-2) on the central nervous system.
The study reveals that SARS-CoV-2 can attack cortical organs and establish infectivity when they are integrated with pericyte-like cells. The study is currently available on the bioRxiv * preprint server.
Background
Coronavirus 2 of severe respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent for coronavirus disease 2019 (COVID-19), is a coated RNA virus that specifically affects both respiratory and respiratory tracts. lower. However, in many cases of COVID-19, SARS-CoV-2 has been found to significantly affect other vital organs, including the heart, kidneys, gastrointestinal tract, and the brain.
Many patients with severe COVID-19 crisis have been found to present with severe brain disorders, including ischemic stroke, seizures, encephalopathy, encephalitis-meningitis, neuro-vasculopathy, and hemorrhages .
Because SARS-CoV-2 enters host cells through angiotensin-converting enzyme 2 (ACE2), it is believed that pericytes derived from neural stem cells express levels well. high of ACE2 as the main brain entry point of SARS-CoV-2. Brain pericytes are perivascular cells that connect endothelial cells with astrocytic cells and regulate important functions of the central nervous system, such as neurogenesis and neuronal degeneration, neuroinflammation, and blood-brain barrier permeability.
In the current study, the scientists are aiming to study whether brain pericytes are susceptible to SARS-CoV-2 infection.
SARS-CoV-2 genetically affects pericyte-like cells.
Study design
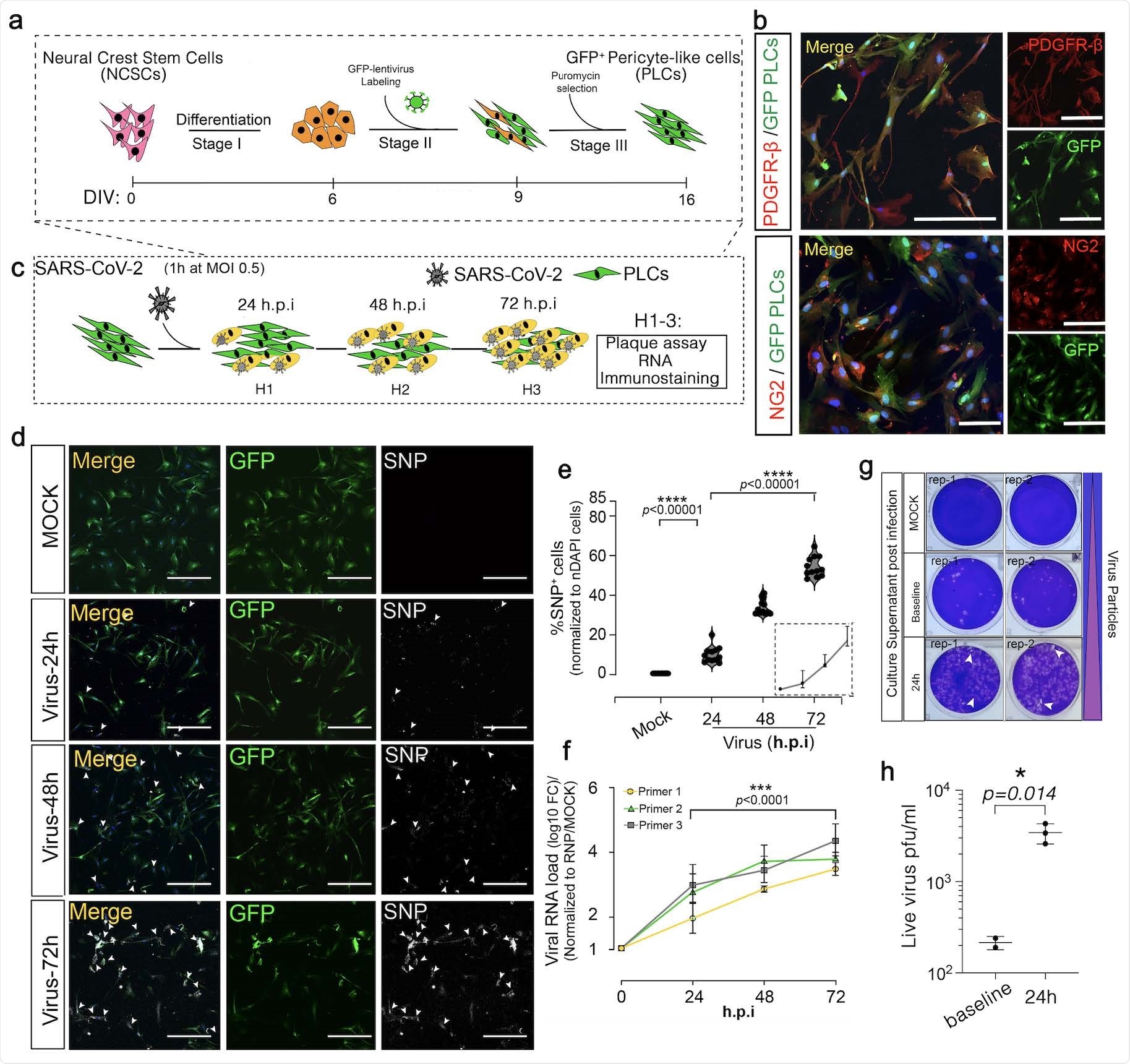
Using in vitro setups, the scientists generated pericyte-like cells from pluripotent gas-coded stem cells. They observed that the pericyte-like cells expressed a very high level of ACE2 receptors. The next pericyte-like open cells with SARS-CoV-2 observed a gradual increase in viral RNA and nucleocapsid-positive viral cells up to 72 h after infection to study transmission dynamics. In addition, they estimated that the production of SARS-CoV-2 became almost 100-fold infectious after 24 hours of infection.
Drawing these conclusions, the scientists studied whether brain pericytes serve as an entry point for SARS-CoV-2 to the central nervous system. They connected pericyte-like cells into mature cortical brain organoids, which are three-dimensional cultures of different brain cells used as an experimental model for human cerebral cortex development. Performing a series of experiments, they confirmed that pericyte-like cells within cortical organs were localized along with astrocytes and embedded within the basement membrane.
When they exposed a cell-like pericyte-like cortical organ to SARS-CoV-2, they observed significantly higher levels of nucleocapsid-positive cells and viral RNA. In contrast, less robust disease has been observed as a result of direct exposure of cortical organoids to SARS-CoV-2. Importantly, they observed that in pericyte-like cortical organs, which contained cortical cells, nucleocapsid-positive cells were co-localized with pericyte-like cells and astrocytes, but not to neurons. Using confocal images, they found that astrocytes themselves were infected with the virus and were localized near pericyte-like cells. These observations indicate that SARS-CoV-2 affects astrocytes through pericyte-like cells.
Regarding the pathogenesis of SARS-CoV-2, they observed a massive induction of neuronal cell death in cortical organoids containing pericyte-like cells. In addition, increased transcription of several type I-induced interferon genes was observed, indicating a higher inflammatory response of type I interferon in cortical organs containing SARS-CoV-2-like cells.
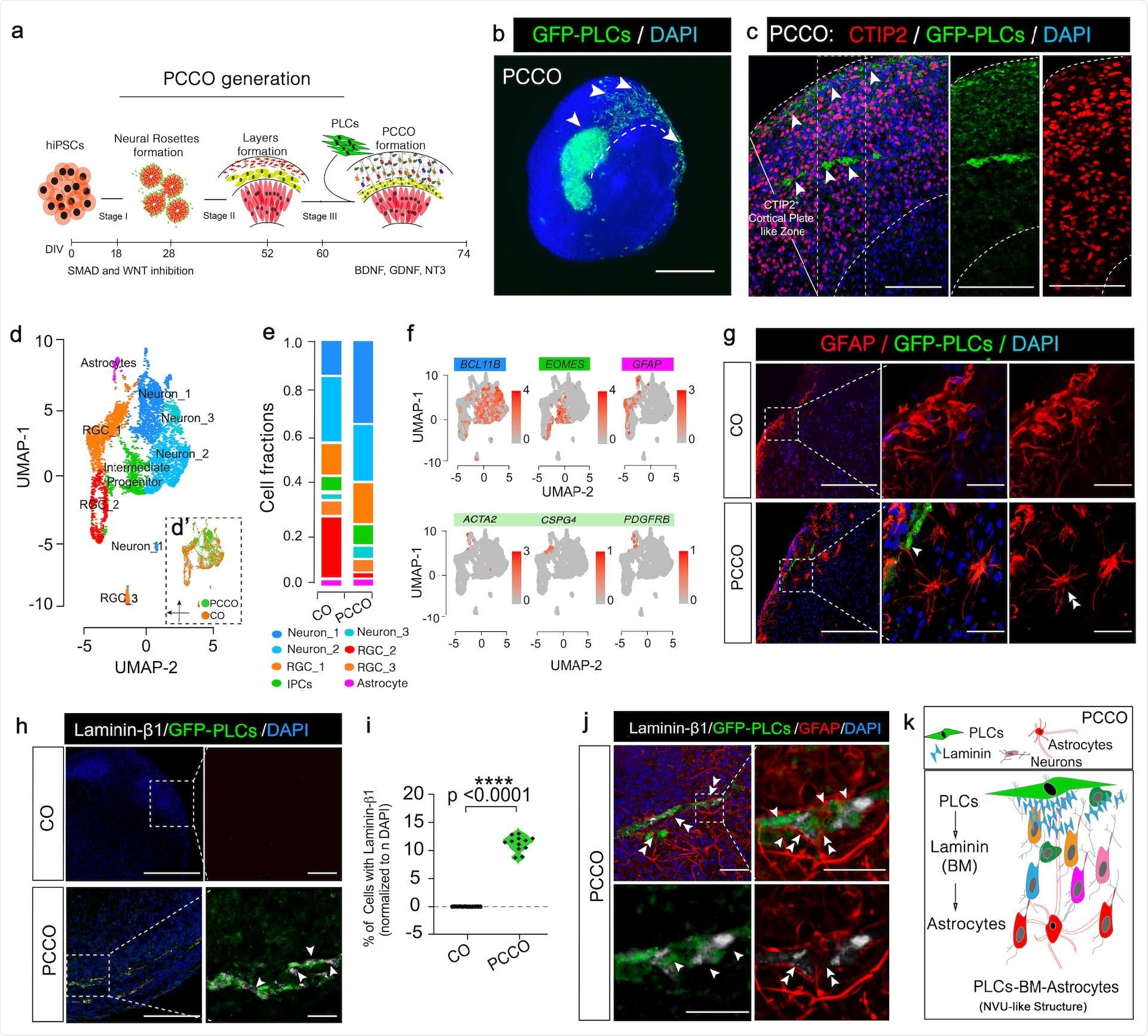
PCCOs inject pericyte-like cells into cortical organoids.
Investigate meaning
The study concludes that SARS-CoV-2 can capture pericyte-like cells and that the vulnerability of cortical organoids to viral infection can be greatly increased by their association with pericyte-like cells. The virus-like pericyte-infected cells can spread the disease to other types of brain cells, including astrocytes. Activation of type I interferon responses and induction of neuronal cell death are critical pathogenic responses observed in cortical organs containing SARS-CoV-2-like cells.
The scientists believe that the organoid cortical model they developed may be instrumental in studying the pathogenesis of SARS-CoV-2 in the central nervous system.
* Important message
bioRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.