Older adults and those with underlying health conditions are at higher risk of developing severe coronavirus infection (COVID-19), the disease caused by the true infectious agent of coronavirus respiratory syndrome 2 (SARS-CoV). -2).
Previous studies have shown that older people are at higher risk of COVID-19 due to physiological changes associated with aging and potential comorbidities, including illness. diabetes, hip tension, and heart problems.
Researchers at the University of California, Irvine aimed to test the differences between young people and older adults in terms of their host responses against SARS-CoV-2. The team showed that COVID-19, which was independent of disease anxiety, was associated with a large shift in plasma inflammatory factors. The search is posted to the pre-print server medRxiv*.
Aging and protective response
The effects of aging on the immune system appear at several stages, including reduced production of T lymphocytes (T cells) and B lymphocytes (B cells) in the bone marrow and the thymus and reduced function of mature lymphocytes or white blood cells.
Many respiratory viral illnesses afflict older adults with severe illness, including the current COVID-19 pandemic, which has affected more than 104 million people. take. More than 2.26 million have contracted the viral disease.
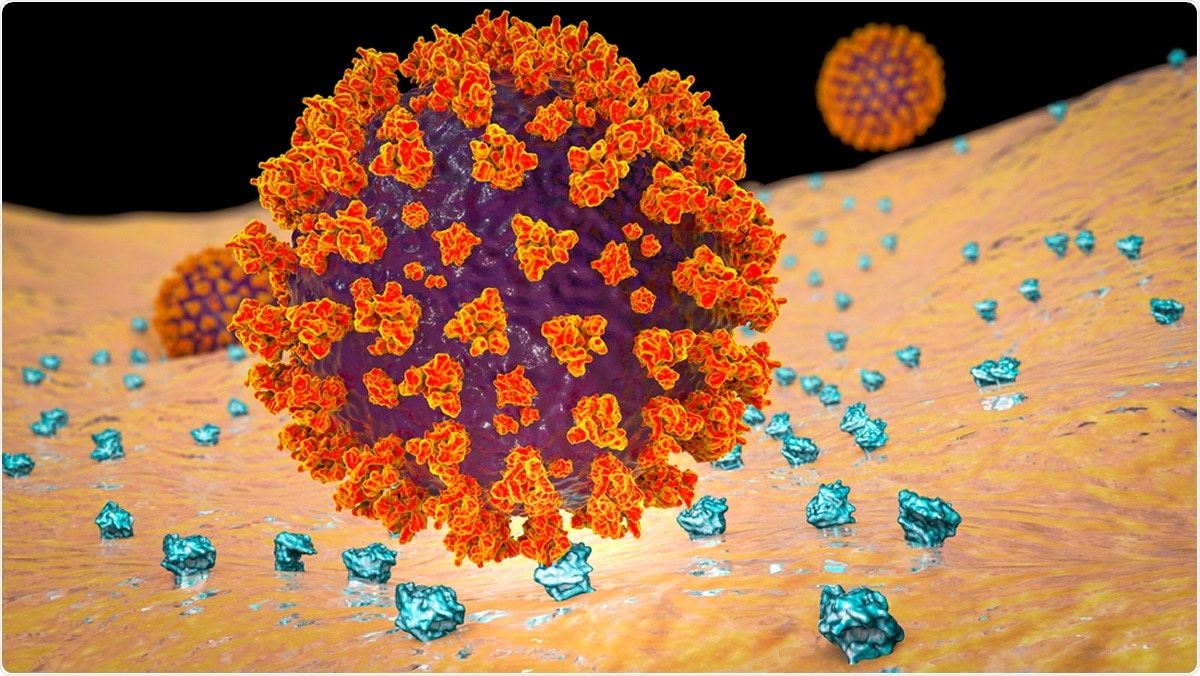
When a person is exposed to SARS-CoV-2, the virus targets the airways of the lungs and alveolar epithelial cells, macrophages in the lung, and vascular endothelial cells. The disease triggers a strong internal and adaptive immune response to eradicate the virus. In more severe cases, the immune system goes out of control, triggering a cytokine storm. Most people with severe COVID-19 develop severe respiratory distress syndrome (ARDS) and multi-organ failure.
In the United States, the estimated mortality rate of COVID-19 is about 1 to 2 percent, while 40 to 80 percent of patients develop only mild symptoms or none at all. Age is a major risk factor for developing severe COVID-19, but more data are needed to explain why this group is predisposed to pandemic disease.
The elderly are the most likely to develop severe complications associated with COVID-19, including respiratory failure, shortness of breath, pneumonia, and ARDS. Further, aging is linked to immunosenescence, leading to a significant increase in vulnerability to respiratory viral diseases, increased inflammation at baseline, also known as ‘inflammaging,’ and response weakened vaccine. Aging is also associated with reduced T cells and B cells, increased circulatory mediators such as interleukin-6 (IL-6) and C 21 reactive proteins and more affective memory cells.
Effect of aging on guest response to COVID-19
The study includes new insights into the impact of aging on the host response to SARS-CoV-2 infection. The researchers conducted the study to find out the differences between young and older people when it comes to how their immune systems fight off the SARS-CoV-2 threat.
It is estimated that approximately 80 percent of COVID-19 deaths are seen among people older than 65 years. People with comorbidities are also at higher risk of serious illness, and most older people have these basic health conditions.
The researchers studied transcription and phenotypic activity of the peripheral mononuclear cells to reach the conclusions of the study. They collected blood samples from patients admitted to the University of California Irvine Medical Center (UCIMC) and participated in the ACT-1 National Institutes of Health (NIH) ACT test. The team stratified the blood samples according to disease severity, including healthy donors, mild or moderate COVID-19, and solid COVID-19.
Age was also considered a factor, where those under 60 are younger, and those over 60 years old. Patients with asymptomatic and mild illness were identified as those with a positive SARS-CoV-2 result for reasons unrelated to COVID-19 symptoms, including elective surgery, heart attack, and autoimmune disease. defense, among others.
At the same time, critically ill patients were reported, including patients who had to be hospitalized or admitted to the intensive care unit (ICU). Their blood samples were collected long over several days after the onset of the symptom.
The researchers collected the whole blood samples in EDTA vacutainer tubes, while peripheral blood mononuclear cells (PBMC) and blood plasma samples were isolated. The team used the XLix Cytokine Discovery Premixed Kit to measure immune mediators, which can test for cytokines, chemokines, growth factors, and affector molecules.
Other experiments included an enzyme-linked immunosorbent assay (ELISA), a single-cell RNA sequence, and PBMC and monocyte immunophenotyping.
The researchers performed a combination of immunological assessments, single-cell transcription, and function using blood samples from 49 healthy donors, 20 mild or asymptomatic COVID-19 patients, and 47 very ill COVID-19 patients with COVID-19. , with long-term sampling based on 10 days post-onset symptom (DPS).
The results of the study showed that there is profound lymphopenia in elderly patients, where there are lower levels of white blood cells, including B cells, T cells, and natural killer cells (NK cells). The lymphopenia worsened over time and is associated with lower levels of plasma cytokines, which are viral for T cell survival in elderly patients with severe disease.
Further, the single-cell RNA sequence showed enhanced activity, cytotoxicity, exhaustion, and type-1 interferon signals in T-memory cells and NK cells. Even though cytokine storms are seen in healthy and age groups, older adults showed higher levels of chemokines that stimulate inflammatory myeloid cells. Finally, the team looked at the recurrence of dendritic cells (DC) and monocytes with severe disease linked to relapse toward a more regulated phenotype.
The team concluded that many of these critical changes in the body and immune system were reversed in younger people, but not in the elderly.
The researchers recommend future studies to confirm young and old patients with clinical scores. In this way, the indications for disease resolution and survival in severe COVID-19 patients can be identified.
“More importantly, addressing the impact of age on qualitative differences in humoral responses and long-term survival of T cell responses to SARS-CoV-2 would be critical in designing vaccination and treatment strategies in the population. age, ”the researchers concluded.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.