.jpg)
New research shows further evidence between COVID-19 infection and the development of long-term brain symptoms. The findings found that neuroinflammation with COVID and microvascular injury contributed to depression-like symptoms. However, they also found evidence revealing a low potential for acute respiratory coronavirus 2 (SARS-CoV-2) direct attack on the brain.
Some people with COVID-19 infection get persistent symptoms – even when the virus has been cleared from the body. An obvious sign of ‘long-COVID’ is brain fog, where people have a hard time thinking and climbing. The current findings could further provide scientists with a greater understanding of the neurological symptoms associated with COVID.
The study “Network therapy links SARS-CoV-2 / COVID-19 infection to microbial brain injury and neuroinflammation in depressive-like brain impairment” is available as a preview of the bioRxiv* server, while the article is under peer review.
Network-based multivariate omics analysis methodology
Study design
The researchers used a protein-protein interaction and CRISPR-Cas9 genetic mutation assay to construct a network-based multivariate viral interaction of SARS-CoV-2. They then examined COVID-19-related cognitive deficits by evaluating transcriptomic images using single-cell and nucleic RNA sequence for Alzheimer’s disease signaling genes in people with COVID-19 disease. Areas exposed to SARS-CoV-2 ingestion in patients with previously undiagnosed Alzheimer’s disease were also studied.
The team assumed that the neurological problems stem from the detection of SARS-CoV-2 host cell genes and proteins in the human protein-to-protein interaction (PPI) network. And they could target the most vulnerable genes and proteins to disease or indirectly through PPI.
Altered Alzheimer’s-related protein and gene modification
Based on the results of PPI and CRISPR-Cas9 genetic evaluations, the researchers found that SARS-CoV-2 host proteins and genes had a significant effect on the expression of Alzheimer’s-related proteins and genes. The modified proteins included RAB7A, TGFB1, and VCAM1.
Low chance of SARS-CoV-2 directly attacks the brain
The team also showed whether SARS-CoV-2 directly affects the brain. They observed the expression of SARS-CoV-2 induction in cigarettes, brain regions, and several brain cells.
Both brain and neurons had low levels of ACE2 and TMPRSS2. In contrast, BSG, NRP1, and FURIN increased the expression in endothelial cells in the prefrontal cortex in Alzheimer’s brain and healthy controls.
“Our findings suggest that SARS-CoV-2 is unlikely to target neurons directly through ACE2. However, we cannot rule out that SARS-CoV- 2 enter the brain through the cerebral endothelium using receptors such as BSG and NRP1 or other unknown entry factors, ”the researchers wrote.
Inflammation of the brain found in patients with COVID-19 infection
Because neuroinflammation is a common symptom of Alzheimer’s disease, the researchers tried to find out if this also occurred in patients with SARS-CoV-2. When measuring symptoms in the blood and cerebrospinal fluid of patients with COVID-19 infection, they found genetic changes – in NKTR, GSTM3, TGFB1, TNFRSF1B, SPP1, and CXCL10 – that have been linked to Alzheimer’s. Endothelial cells also had increased expression of the following antiviral immune genes: LY6E, IFITM2, IFITM3, and IFNAR1. The STAT3 and JAK1 genes appear to play a role in neuroinflammation, which is consistent with previous studies affecting the JAK-STAT signaling pathway in exacerbating COVID-19 symptoms.
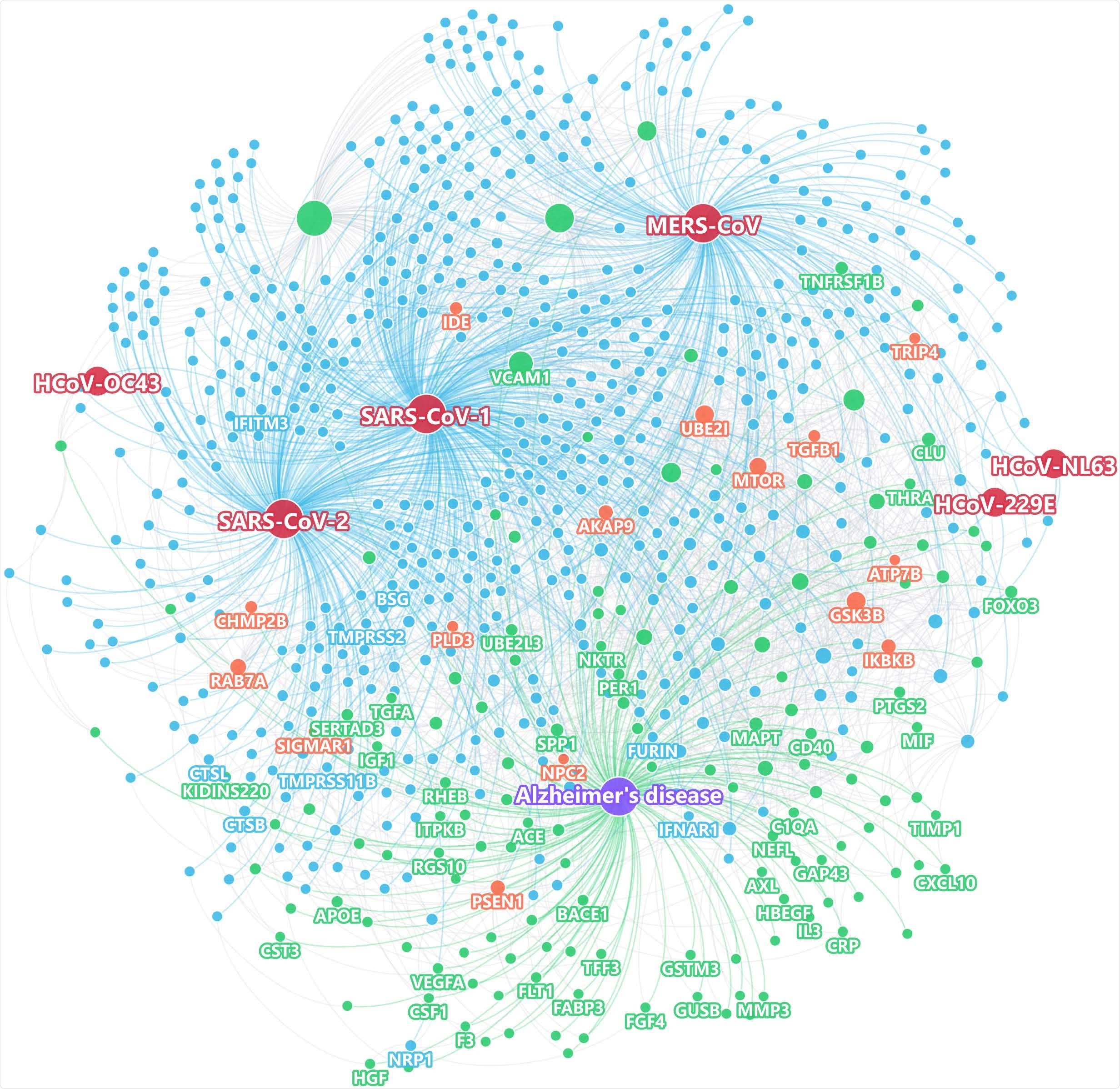
Using measures close to a modern network to evaluate the network-based relationship for the gene / protein sets between virus host factors and each disease / condition under the human interactive network model.
People with APOE E4 / E4 show lower expression of antiviral immune genes than people with the APOE E3 / E3 gene, showing a lack of gene expression and an increased risk for COVID-19 disease. The researchers suggest more studies looking at the association between APOE gene expression and the likelihood of developing SARS-CoV-2 disease.
Explore boundaries to consider
Despite using high-quality data from multiple sources, the researchers acknowledge that their human-protein interactions are infinite, revealing the potential for network associations to be either positive or negative. Also, the researchers found low sensitivity of ACE2 and TMPRSS2 but were unable to rule out access to another key SARS-CoV-2 entry factor. Another limitation was that the current study did not evaluate potential neuroinflammation pathways in patients with both Alzheimer’s and COVID-19, which may have influenced the findings.
“The importance of our decisions in the context of the general population of COVID-19 often suffering from“ brain fog ”without a formal diagnosis of AD requires further study,” the research team concluded.
* Important message
bioRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.