The introduction of vaccines against coronavirus 2 (SARS-CoV-2) has long been introduced, with several vaccines approved in the USA, Europe and Asia. However, vaccine supply remains limited, making it necessary to strategically plan vaccine circulation over large populations.
Thoughtful preview research paper posted to medRxiv* the server suggests that, among a number of factors that may contribute to the design of an optimal vaccination strategy aimed at minimizing the potential for COVID-19 mortality, it seems that time is of the essence.
Current situation in the USA
The first two vaccines approved for emergency use by the U.S. Food and Drug Administration (FDA) were the Moderna and Pfizer-BioNTech vaccines, which are reported to have more than 94% efficacy in preventing symptomatic disease. COVID-19. Priority has been given to frontline and other high risk personnel, a priority vaccination schedule has been introduced.
Of the nearly 30 million doses dispensed among the states, about 10 million had been administered by January 13, 2021. In the current study, the researchers modeled the effect of vaccine distribution at different times, in several priority orders, and in single vs double dose governments, in terms of population level mortality. The model was based on age and risk parameters.
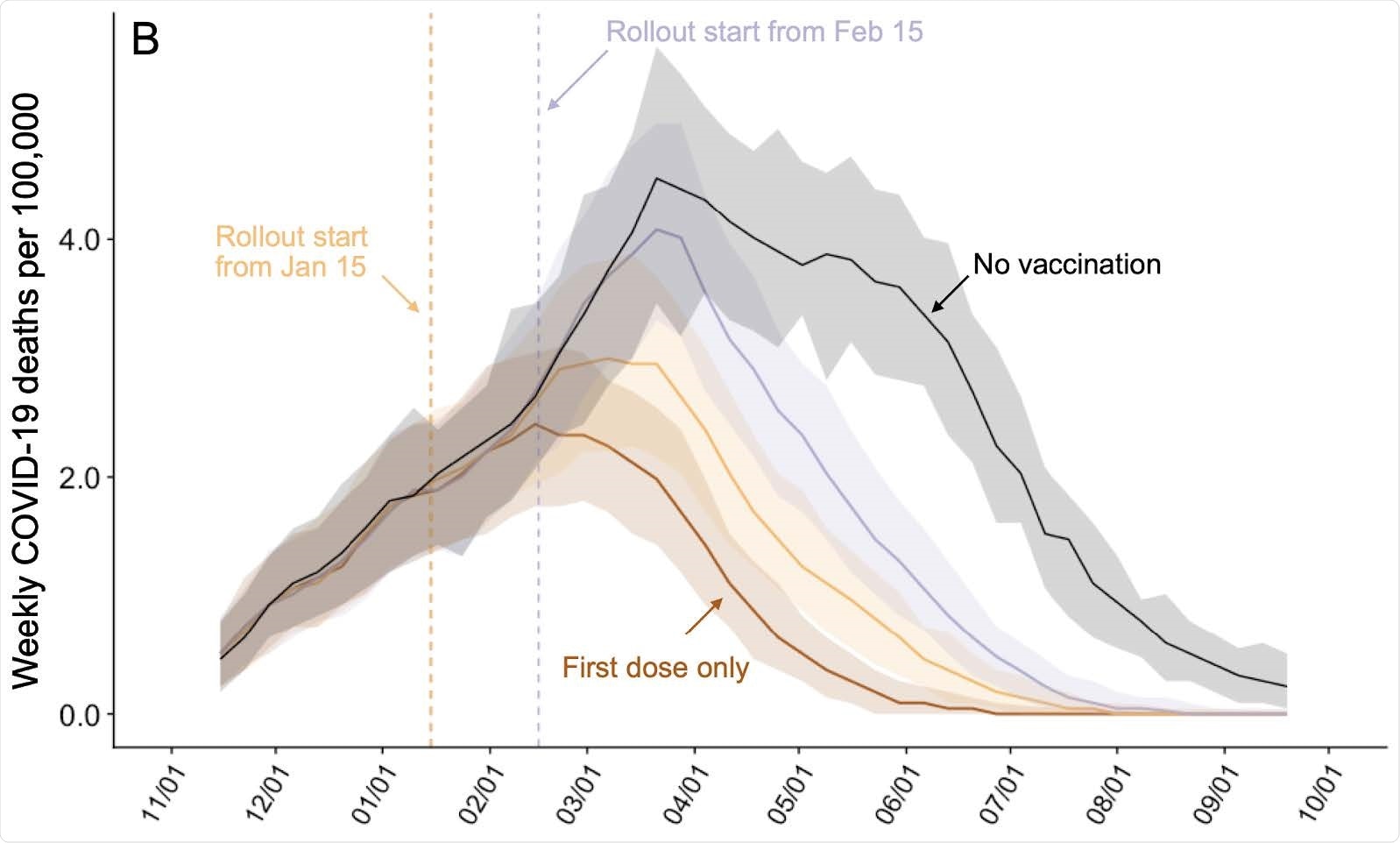
Projected mortality of COVID-19 in MSA Austin-Round Rock from November 8, 2020 to September 17, 2021 under different conditions of vaccine distribution. Weekly incidence of COVID-19 deaths per 100,000 assuming intermediate uptake (70%) (9) without vaccination (black) or under ten-dose spread based on a 95% risk of 95% effective infectious prevention, starting either January 15 (orange) or February 15 (purple). The brown line assumes that only first doses are administered starting January 15. Solid and blackened lines indicate a mean and 95% CI over 200 stochastic samples, respectively.
Study model
The study model was based in Austin, a Texas city, with the number of COVID-19 deaths projected over eight months after two types of vaccine were used: one that prevents infection with making the vaccinated less susceptible, and the other focusing on a symbolic disease. The study is based on the assumption that the vaccine is leaking, resulting in a 95% reduction in vulnerability.
The deadline for vaccine distribution is January 15 or February 15, and the weekly vaccine quota is estimated at 10 million. Vaccination distribution to each city is on a pro-rata or proportional basis.
The model compared three strategies, one of which is to spread the vaccine as they come; one that prioritises three groups before getting the vaccine available to the general public, namely, those over the age of 65, those with high – risk medical conditions, or both; and a ten-step strategy with continued administration of the vaccine to at-risk-of-age groups at risk of developing adverse effects of COVID-19. The study assumes that approximately 8% of individuals have become immune after a natural infection by this date.
Vaccine that prevents disease
Third, by adhering to a perfect risk prioritization in vaccine delivery, with a vaccine that prevents infection, the researchers estimate a 52% reduction in deaths due to COVID-19 compared to controls. unvaccinated if 50% of the population is vaccinated. If 90% coverage is achieved, 56% of deaths will be prevented.
If coverage is low, i.e., 50%, priority-based vaccination is largely inappropriate. At 90% or more coverage, the ten-level strategy is preferable first, followed by those over 65, and young adults at high risk.
Symbolic infectious prevention vaccine
With a vaccine that simply blocks a symbolic disease, the 50% coverage effect is estimated to begin on January 15, using the ten-tier strategy, able to reduce the death toll by 40%, compared to 32% with nonprogrammed pre-distribution strategies. . Osbarr the coverage is under the 89% ten-dose strategy with a single dose. In that case, the estimated reduction is 50% and 66%, respectively, for a vaccine that simply blocks a symbolic disease and one that prevents infection as well.
With these decisions as a basis, high-risk groups should be prioritized. With a delay in transmission in February 2021, with only 50% uptake, giving the vaccine to those over 65 and those at high risk can prevent around 17,000 more deaths than non-priority schedule.
Delay in deployment is the most lethal parameter
On the other hand, the only factor associated with a higher number of deaths in the US and Europe is a delay in vaccine distribution, compared to poorly prepared or implemented priority plans the action or willingness to take the vaccine.
At present, thousands of deaths occur every day in these countries. As new changes begin to take over in many of these areas, with even more movement, the process of making sure the vaccine reaches people who are susceptible to it before the virus takes on the biggest challenge. This is more because, in contrast to seasonal prevention campaigns, which occur before the flu virus begins to circulate freely, the COVID-19 vaccine appears at a stage where the causative virus, syndrome. acute acute coronavirus 2 (SARS-CoV- 2), already in full cry.
One-dose extended programs
Some vaccine programs have chosen to extend the reach of the first dose of the vaccine rather than complete the two-dose regimen in as many people as possible. It is hoped that the partial protection afforded by the first dose will still be more effective in reducing the number of deaths, compared to having a much higher immunity in half the number of people.
However, the US has expressed disagreement with this approach, because there were no clinical trial data demonstrating one-dose convenience. It is against this background that the current study models a situation where giving just one dose of each type of vaccine, at 80% efficacy, would prevent more deaths than requiring two doses for each participant.
What is the impact?
The researchers argue that more information needs to be gathered about the effectiveness of vaccines after single-dose trials as more assumptions are made about the type of onset, duration of immunity, and outcome of the vaccine. finally, whether it is infection prevention, symptomatic disease or any combination of both. The actual performance of the model also depends on the proportion exposed to the population, the changes in the behavior of the people over time or after the vaccination,
However, the study strongly recommends that the release of priority vaccines should not delay distribution, as seen in the US.
The researchers describe their plan: “Our projections recommend two immediate strategies to increase the impact of COVID-19 vaccines in the US –– hybrid releases that combine active access to priority groups with passive public distribution and previous plans to keep second doses in reserve.. ”
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.