Researchers in Italy have conducted a study showing that patients who tested positive for infection with severe acute respiratory coronavirus 2 (SARS-CoV-2) syndrome were still neutralizing antibodies against the virus 10 months later. after that.
SARS-CoV-2 is the agent responsible for the 2019 coronavirus pandemic (COVID-19) pandemic that remains a global public health threat and has now claimed the lives of more than 2.49 million people.
The researchers evaluated antibody responses over 10 months among 30 people diagnosed with SARS-CoV-2 infection in the Umbria region of Italy between 1st and 30th March 2020.
At ten months after infection, 19 (63%) of the individuals still had detectable levels of immunoglobulin G (IgG) antibodies neutralized against SARS-CoV-2.
Moreover, no recurrence case occurred among any of the participants, despite an increase in daily infections with mutant sequences occurring in the Umbria region during the study period.
A pre-printed version of the research paper can be found on the medRxiv* server, while the article is subject to peer review.
Concerns about antibody responses to SARS-CoV-2
Since the COVID-19 revolution began in Wuhan, China, in late December 2019, studies have shown that low antibody responses among recovered patients can last anywhere from three months. to more than eight months.
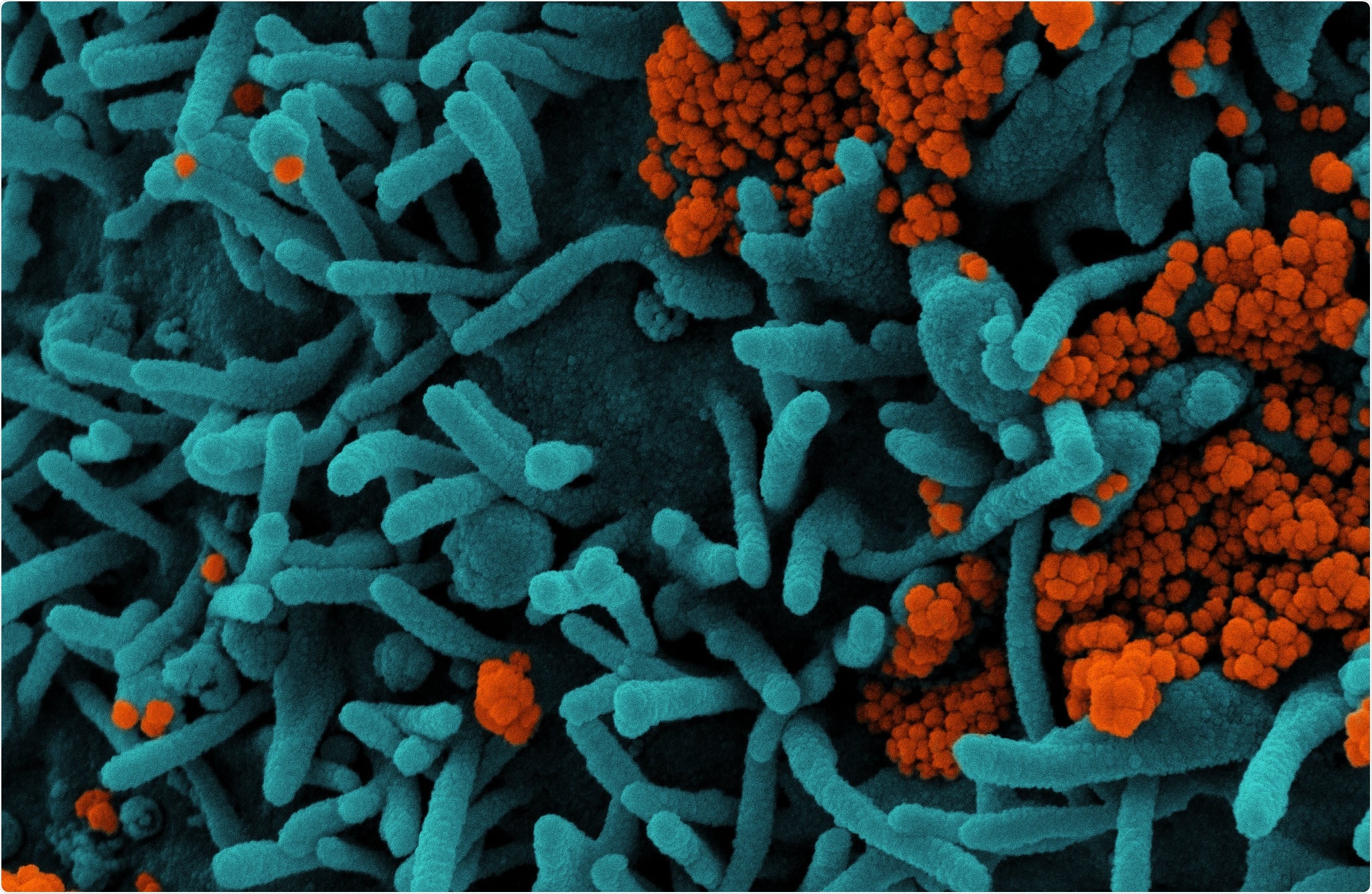
The SARS-CoV-2 virus secretes four major structural proteins, among which the spike protein (S) and nucleocapsid protein (N) are the most immune.
The spike protein is the main structure used by the virus to bind to and enter host cells.
As the first stage of the infectious process, the spike binds to the host cell receptor angiotensin-converting enzyme 2 (ACE-2) through its receptor binding domain (RBD).
The RBD spike is the primary target of SARS-CoV-2 neutralizing antibodies, which are detected as early as six days after diagnosis of polymerase chain reaction (PCR) infection.
Studies published in 2020 have raised concerns about the length of immunity provided by these neutral antibodies, warning that “rapidly declining immunity” could lead to false-negative immunoassay results.
“A better understanding of immunity offered by the antibodies developed against SARS-CoV-2 is essential,” wrote Puya Dehgani-Mobaraki of Associazione Naso Sano in Umbria, Italy and colleagues.
What did the researchers do?
The researchers performed a long-term observational analysis of 114 patients in the Umbria region who had tested positive for SARS-CoV-2 with real-time quantitative PCR between 1st and 30th March.
They conducted series of trials over ten months among 30 of the participants who attended all follow-up rounds.
Blood samples were collected at six different points (T), with the first sample taken two months after infection in May (T0). Further samples were then taken one month (T1), three months (T2), five months (T3), six months (T4) and eight months (T5) after T0.
The presence and persistence of specific SARS-CoV-2 antibodies was assessed using two commercial chemiluminescence immunoassays (CLIAs), with a favorable CLIA cutoff set at> 1.01.
Participants were divided into those with moderate-to-severe disease (n = 17) and those with moderate-to-severe disease (n = 13).
What did the study find?
The team reports that anti-spike-RBD IgG was detected in 19 (63.3%) of the 30 participants at T5 – ten months after first being diagnosed with an infection.
Among both the mild disease group and the moderate-to-severe disease group the movement of SAR-CoV-2-specifc IgM titers remained below the CLIA (> 1.01) positivity cutoff and decreased significantly over the ten months.
In contrast, IgG titer movement remained above the CLIA favorable expectation in both groups and no significant changes in titer were observed.
Furthermore, “our study reported zero cases of relapse despite the fact that the Umbria region is currently experiencing an increase in day-to-day cases with mutant sequences,” the team concluded.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.