Researchers tested several RNA collection and extraction methods and evaluations to develop a protocol for testing SARS-CoV-2 in wastewater, which may help improve COVID-19 sensitivity.
COVID-19, caused by the acute respiratory coronavirus 2 (SARS-CoV-2) syndrome is usually monitored by finding sympathetic patients and locating their identities. However, this may not be entirely correct as it requires voluntary individual involvement and does not involve asymptomatic cases, making it challenging to control transmission.
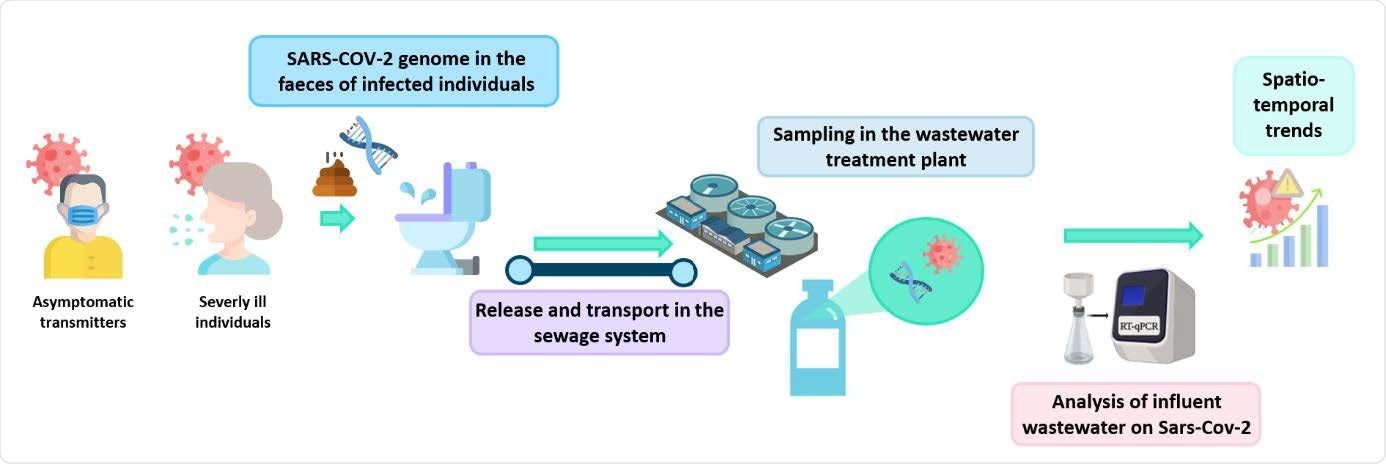
Wastewater testing is another way to monitor the spread and circulation of infectious diseases. Symptoms of disease such as viral genomes are released and carried in the wastewater. The abundance of pathogens in wastewater can be used to detect the spread of disease.
Several studies have reported the use of wastewater to monitor the spread of SARS-CoV-2. However, there are some challenges in doing this. Because wastewater contains a lot of organic matter and other metals, it can be difficult to detect low virus levels. Furthermore, it is not known with certainty what form the SARS-CoV-2 virus is present in feces, such as virus particles, fragments and so on, which may be broken down. down further when wastewater is transported. Therefore, it is essential to have reliable methods for targeting and detecting viruses.
Testing strategies
In a research paper published on the medRxiv * preprint server, Belgian researchers report a comparison of different bioanalytical methods for SARS-CoV-2 RNA concentration in wastewater.
An overview of sewage study to determine the circulation of SARS-CoV-2 in the general population.
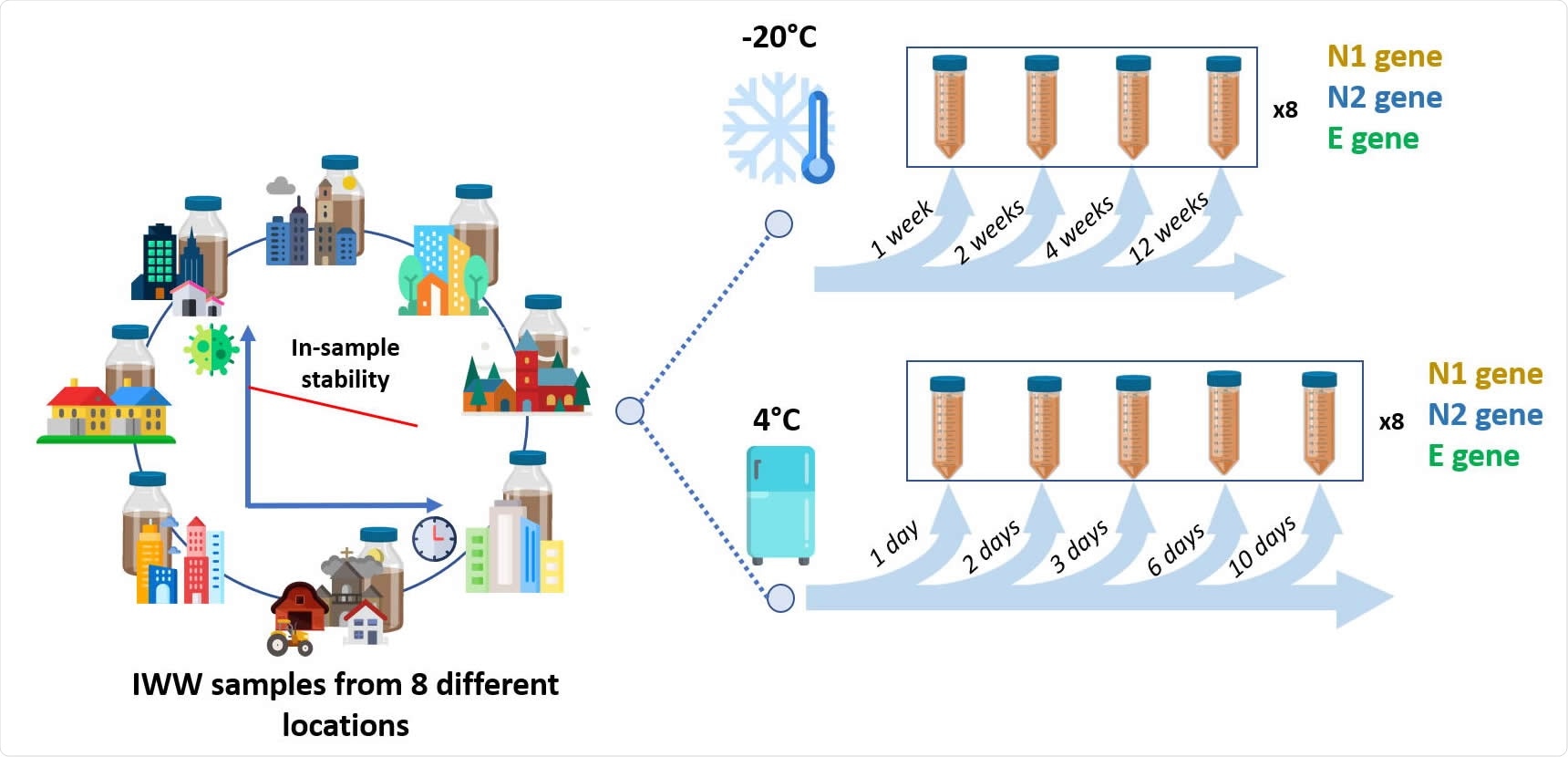
The team obtained wastewater samples from eight wastewater treatment plants in Belgium and sanitary wastewater from a company that had a high number of COVID-19 cases. They used various ultrafiltration methods using several centrifugation devices and polyethylene glycol (PEG) precipitation to target viral RNA. The method that provided the lowest and most reproducible levels of cycling threshold (Ct) for SARS-CoV-2 gene amplification was used for sample density.
The team also tested several commercial RNA extraction tools to select the one that gave the lowest and most reproducible Ct values. They used both RT-PCR and digital PCR (dPCR) for amplification of viral RNA. DPCR may be more useful for wastewater testing because it is less sensitive to PCR inhibitors present in wastewater and provides total volume.
Improved analysis protocols
Based on the collection results for samples collected in August 2020, when the number of cases was lower compared to those in the second wave, the team found that PEG leakage could not detect N1 and N2 genes and concentrations of swine coronavirus were significantly lower. Therefore, this approach was no longer followed.
When tested for the effect of different filter pore sizes and sample sizes, the team found that while smaller sample pore sizes may have improved, they often resulted in filter blockage and a density of protectors. PCR. Therefore, they used a molecular weight cutter of 50 to 100 kDa and a sample volume of 50 to 500 mL. Viral levels were too low to detect without density. A collection step was therefore required to detect SARS-CoV-2 in wastewater. In the last protocol, the researchers used ultracentrifugation with Centricon filters.
Although both the manual method of RNA extraction and the automated method used the Maxwell PureFood and GMO test kit compared for RNA extraction, the team chose the automated method for the high throughput.
The authors found that both RT-PCR and dPCR yielded the same aggregation levels, indicating that the sensitivity of the two assays is similar. However, the advantage of a dPCR is that it does not require a standard loop.
When water is carried in the sewage system, the SARS-CoV-2 genome can be broken down into smaller RNA particles. The team found that tested N2 and E genes were above the minimum measurement level for more than 87.5% of the wastewater samples. However, there was a difference in the E gene with time. Given that there was a significant difference in the indigenous assemblage at the lowest measurement level, assessing sustainability is a challenge.
Frozen samples reduced 10-fold gene copies, but detection rates were higher in samples kept at 4 ° C. The authors recommend keeping samples at this temperature and examining them separately. within three days of collection.
Despite the development of better protocols, there is still considerable variation in sample collection methods as there is no external standard for comparison. Also, the state of the SARS-CoV-2 genome in wastewater is highly uncertain due to potential contamination in the sewage system. Further research is needed to better understand these variables and their potential use in wastewater-based epidemiology for SARS-CoV-2 study.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.