
A.s Margaret Keenan, 90, was being discharged from Coventry University Hospital this month, hand in hand with her daughter and granddaughter, carrying a newspaper with the headline: “ One small kick for Maggie, one big jump for us all. ”
“You are so famous that they compare you to the astronauts who walked on the moon! ”Asked one nurse.
The day before, at 6.31am, Keenan was the first clinical patient in the world to receive the first dose of the Pfizer / BioNTech Covid-19 vaccine. “Yesterday was a great day for me and the rest of the world as we all look back to some sort of routine,” she said.
When she left the hospital, goodbye recognized her and congratulated them. The vial and syringe used in her innovative vaccine have been donated to the Science Museum in London for future reference.


-
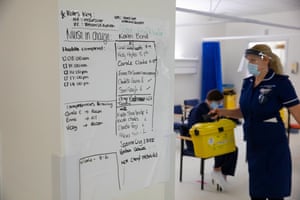
Margaret Keenan, 90, was the first patient in the United Kingdom to receive the Pfizer / BioNTech Covid-19 vaccine. She left the hospital with her daughter and granddaughter. All pictures by Jonny Weeks
The university hospital, part of the Coventry & Warwickshire University Hospitals (UHCW) trust, is one of about 70 hospitals across the UK participating in the vaccine rollout. The first priority is given to people over 80, care home staff and vulnerable NHS staff. Every day, around 300 people receive the vaccine in a University hospital alone.
Mark Easter, pharmacy director, oversees storage and delivery. “The vaccine needs to be stored at -60C to -80C and we usually don’t have freezers like this in the pharmacy, so we had to put one in,” he said.
His colleague Santosh Kalair, with thick, waterproof gloves and a gown, opened the freezer door to discover what is known as a 195-box “pizza box”.



“It’s a new drug and it’s very fragile, so we can’t keep the door open for 43 seconds,” said Easter. “We have to take it out and disinfect it for three hours in the fridge on a Saturday night. The nurses then have to reconstitute by adding saline, during which time they have a shelf life of six hours. Once in the syringe, they must be used immediately.
“We have applied for jabs every five minutes from 9am to 4pm, and we repeat that every day. But you are immune only a week after the second dose. The first dose is definitely a primer. ”
Santosh Kalair and May Parsons
May Parsons, who delivered the first injection to Keenan, said: “It was awful because people were watching her every move and reaction, but there were no crooked hands when I saw the pictures. Tbh.
“I was really looking at Maggie. You know when you look at your patient and you think: I just want to make sure she’s okay. It is about taking the patient away from the needle. I squeeze my arm to take the mind off the future. ”



The first hospital staff to receive the vaccine included Candice McGrane, a modern matron, and Bernice Dudkowsky, a consultant in emergency care and anesthesia. McGrane promised with anticipation. “I’m not good with needles considering I’m a nurse, but it was good,” she said.
Dudkowsky said: “Being at the very beginning of anything is always a bit of an element, but someone has to go for it. It was approved and I am personally grateful to have had the opportunity to have the vaccine. If we can protect NHS workers, the elderly and the vulnerable, everyone else can get back to normal. “
Warning: readers may find the images below disturbing
Divider 2

But that hope is diminished by the knowledge that many patients are still very ill. On Oct. 12, there were 25 Covid-positive patients at the University hospital, two of whom were in emergency care. Before Christmas Eve, the numbers 112 and 13 were respectively.
Some patients are sensitive during their time in emergency care. In one bed, a patient needed Cpap (progressive air pressure) to help her breathe. In another bed, a woman gasped as her oxygen mask was removed.
Emergency care consultant Aoife Abbey said: “We have had a number of deaths [in the weeks before Christmas] and we find that the patients who are placed on ventilators are now very ill. It’s sad because most of these patients were pretty good, they were enjoying their previous life.
“In the second wave of the pandemic, the average age of admission is in the early 60s. There are people if it weren’t for coronavirus, they certainly wouldn’t be dead right now. “
She said: “The people I lost recently would not be [qualified for] vaccines still at least. ”




Roger Townsend, former clinical director of emergency care, said changes were made in the second wave of the pandemic to allow compassionate trips for family members.
“I think we got the balance right when we opened the pubs but kept the hospitals closed to visitors,” he said.
“We all agree that a visit is good for patients, their families and staff too, so we should have improved the visiting environment. [sooner] for it has been miserable. It’s much easier for lovers to accept that the treatment doesn’t work when they see that we’ve struggled, that we’ve fought a good fight.
“The first wave was hard to reach and it had to be because we didn’t know where it was going or how much this virus was transmitting; we didn’t want people to come in to visit loved ones and then take it home to their families.
“But people working in emergency care do not appear to be highly susceptible to the virus so it tells us that the PPE [personal protective equipment] we use to work and the environment is a reasonable place to visit. ”

-
Emergency care staff. Top row (lr): Russel De Lara, staff nurse; Jhoan Detubio, clinical sister; Abbey Aoife, councilor; Roddy Daguio, health care assistant; Luke Closs-Parry, physiotherapist. Bottom row (lr): Yesita Putri, young doctor; Roger Townsend, councilor; Tamiru Feyie, staff nurse; Samuel Collier, staff nurse; Michelle Blackstock, staff nurse
Clinical and support staff in emergency care included Tamiru Feyie and Sushma Lapsley. After getting a proper test for the FFP3 mask, Feyie was embarking on his first move just as Lapsley, who has been with the NHS for 42 years, was finishing her last.
“I was going to leave but I stopped to do my part because of Covid,” Lapsley said. “I thought we would sort it out [by now] and there would be fewer patients. But it’s not going to end, is it? ”


-
Tamiru Feyie, a new member of intensive care staff, is undergoing a proper test for the FFP3 mask; Sushma Lapsley congratulates her on her appointment
As Christmas approached, many employees had expressed awareness of the potential impact of five days of social restrictions. There was relief when stricter measures were applied.
Speaking ahead of Christmas, Abbey said: “The restrictions are sad. They will bring with them a lot more economic losses and will mean that some people will spend Christmas as well as lovers. But other festivals have suffered before this one: Diwali and Eid, for example. In all cases there has been sacrifice, but it is absolutely necessary. ”
Commenting on the news of a more widespread Covid series sweeping the south east of England, she said: “The message is welcomed that this new variant is not related to a more serious illness, but the Covid’s possible disease spectrum already produces horrible results so just experience it [up to 70%] it’s more portable enough to bother me. ”


Halfway through her move, Abbey learned that another middle-aged patient with whom she had developed a relationship had died. She was visibly moved and accepted by a colleague.
“The day has been very difficult today but look what I found,” she said. In the palm of her hand, she showed a small card left to her at the patient’s bedside, anonymously offering her moral support.
Read it: “Here is a small pocket cup to keep you safe. Keep it close to your heart and know you love it. “
Abbey said: “My colleagues and I are not robots and we get so much grief and sorrow. That little card didn’t ask if I was okay, it was an acknowledgment of ‘I know this isn’t okay and I’m here with you’, which was so beautiful at the time. ”

Divider 4