Acute myeloid leukemia is a good model for the study of cancer stem cells because 10% –20% of individuals older than 70 develop preleukemic mutations in hematopoietic cells. From here, the preleukemic stem cells can produce healthy blood and immune cells, but the buildup of additional mutations could lead to malignant proliferation of aberrant leukemic gas cells.
These cancer stem cells can stimulate long-term cancer growth with their ability to regenerate continuously. However, low distribution rates make them difficult to target therapeutically. Chemotherapy often destroys the leukemic stem cells, leading to regular recurrence. Therefore, there is an urgent need to identify therapeutic strategies that target leukemic stem cells, while suppressing healthy hematopoietic gas cells.
Researchers from the Center for Genomic Control (CRG) and the European Molecular Biology Laboratory (EMBL) wanted to develop an approach that could identify gene expression differences among healthy hematopoietic stem cells, preleukemia stem cells, and leukemia cells. Together, MutaSeq, augmenting nuclear mutations from component DNA (cDNA), and mitoClone, a computational device that achieves high-resolution clonal specifications and de novo detection of clones using mitochondrial signal mutations when available, let with the team used genomic and mitochondrial mutations to differentiate between healthy cells and cancer.
They measured mutational status and gene expression in single cells simultaneously to differentiate cancer stem cells from both mature cancer cells (based on gene expression) and healthy stem cells (based on mutational status). ). Furthermore, they were able to differentiate preleukemia stem cells by detecting clonal hematopoiesis of indeterminate lesions (CHIP).
To study MutaSeq applications in conjunction with mitoClone, the researchers generated data from four acute myeloid leukemia patients with heterogenous genotypes and phenotypes. The final data set contained 618–1430 cells per patient, of which 190–968 were CD34 + (indicative of acute myeloid leukemia).
The researchers then collect cells into a clonal hierarchy (a descending relationship between the different cells that reflects the order in which mutations were found) based on nuclear genomic mutations, as well as mitochondrial mutations.
This mechanism revealed known preleukemia mutations, such as mutations in the SRSF2 and DNMT3A genes. However, with reliance on somatic nuclear mutations I missed the identification of other mutations with a lower emotion. For them, the team used mitochondrial mutations to update clonal hierarchy along with nuclear mutations. In two of the samples, they found that preleukemic, as well as subclonal leukemic mutations, were significantly associated with specific sets of well-covered mitochondrial changes.
Across the four patients, the researchers identified clones containing known preleukemic mutations (in SRSF2 and DNMT3A) and subclinical cells carrying known leukemic mutations (CEBPA and NPM1).
On a de novo basis, the researchers used MutaSeq to identify clones associated with leukemic stem cells. They found a very important association of splicing mutation 2 (SRSF2) rich serine and arginine spineing with the leukemic and preleukemic subspecies and DNA methyltransferase 3A (DNMT3A) mutation associated with unrelated mutation in the RPL3 gene.

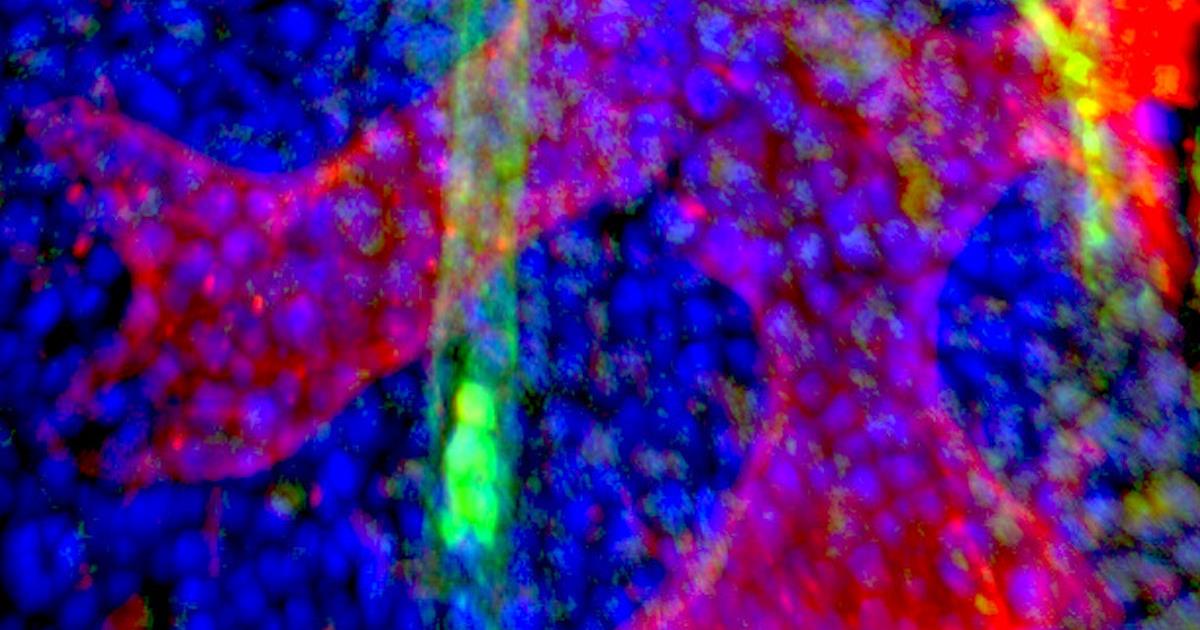
Imaging of gas cells (blue) in bone marrow along with sinusoidal blood vessel (red) and arteriolar blood vessel. Image courtesy of Jude Al-Sabah / DKFZ.
Next, they used single-cell transcription data to differentiate stem cells, progenitor cells, and leukemic eruptions (white blood cells in bone marrow). Transcription factors, such as protein activator 1 (AP1), appear to be relevant in all, significantly different, swelling numbers.
They combined single-cell gene expression data and clonal tracking results to identify characters as (pre-) leukemic cells or healthy cells. Importantly, MutaSeq data allowed gene expression to be compared between different clones in a single mutation. This allowed the researchers to determine the specific effects of a single mutation of hematopoiesis.
Mutations in the de novo methyl transferase DNA, DNMT3A, have been found to be the most common cause of abnormal clonal enlargement of healthy cells in advanced-aged individuals. Also, mutations in the multifactorial ribonucleoprotein 1 (NPM1) have been identified as drivers for acute myeloid leukemia in 30% of patients and often occur with preleukemic DNMT3A mutations.
Finally, the researchers compared gene expression between all (pre-) leukemic and nonleukemic cells, with the aim of identifying potential symptoms or drug targets present in all leukemic (pre-) cells, but not in healthy cells are left.
“There are a large number of small molecular weight drugs out there with proven clinical safety, but it is a daunting task to determine which cancers and in particular which patients these drugs are suitable for. , “the author explained Lars Steinmetz, PhD, a professor at Stanford University and group director at EMBL Heidelberg, in a statement.” Our approach can identify drug targets that may not have been proven in the proper context. These tests need to be done in controlled clinical trials, but knowing what to try is an important first step. “
“We have now brought together clinical researchers from Germany and Spain to apply this approach to much larger clinical studies,” said author Lars Velten, group director at the CRG. “We are also making the method much simpler. Our vision is to identify specific gas cell drug targets in a personalized way, ultimately making it as easy for patients and doctors to find these treatments and which it tests for coronavirus “.
Do you have a particular perspective on your research related to cancer research or genomics? Contact the editor today to learn more.
—
Copyright © 2021 scienceboard.net