A key mystery in Alzheimer’s disease research is why some brain cells adhere to the creeping pathology of the disease years before symptoms first appear, while others look invisible to the decay around them until the late stages of the disease.

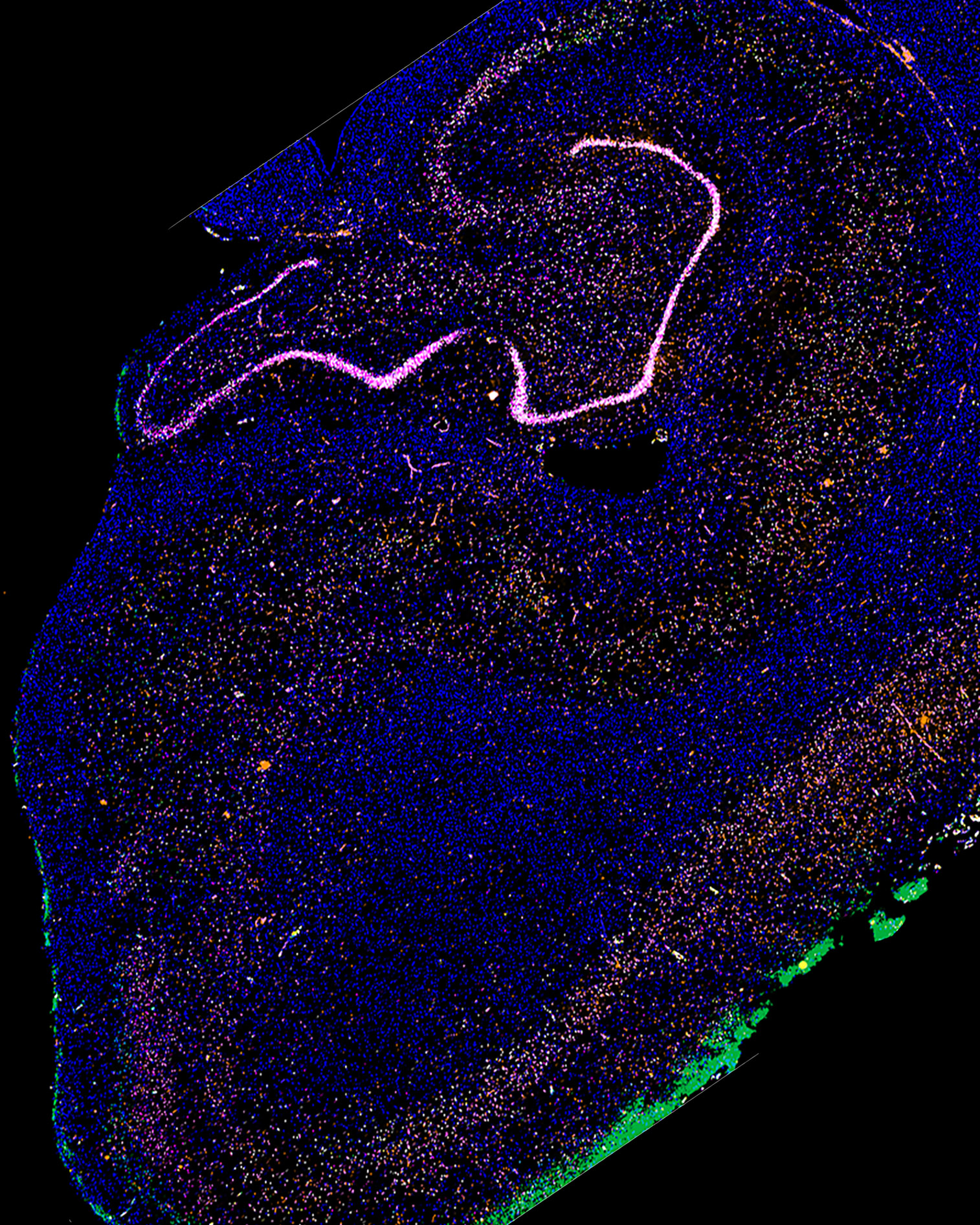
Imaging of human brain samples used to study why some brain cells are more vulnerable to Alzheimer’s disease than others. Image by Rana Eser, UCSF Grinberg laboratory
Now, in a study published Jan. 10, 2021, in Ignorance of nature, a team of molecular biologists and neuropathologists from the UCSF Weill Institute for Neurosciences have come together to identify for the first time who are among the first victims of the disease – collecting toxic “tangles” and die earlier than neighbor cells.
“We know which neurons die first in other neurodegenerative diseases such as Parkinson’s disease and ALS, but not Alzheimer’s,” said co-author Martin Kampmann, PhD, associate professor at the UCSF Institute for Neurodegenerative Diseases and Chan Zuckerberg Biohub Investigator. “If we understood why these neurons are so vulnerable, we might be able to identify interventions that could make them, and the brain as a whole, more resistant to the disease. ”
Alzheimer’s researchers have long studied why some cells are more likely to produce toxic lumps of the protein called tau, which has a transmission through the brain that drives widespread cell death and progressive memory loss, depression, and other symptoms. But researchers have not looked closely at whether all cells are equally vulnerable to the toxic effects of these protein accumulations.
“The belief in the field is that once these waste proteins are in place, it is always a ‘game over’ for the cell, but our laboratory has been getting its that is not true, ”said Lea Grinberg, MD, fellow senior study author, associate professor and John Douglas French Alzheimer’s Foundation Endowment Professor at the UCSF Center for Memory and Aging. “High levels of tau go well in the progression of the disease in some cells, but for some reason they do not die. It has become an important question for us to understand the specific factors that leave some vulnerable cells to Alzheimer’s pathology, and it seems that other cells are able to resist for years, if not decades. ”
To identify vulnerable neurons, the researchers examined brain bones from people who had died at various stages of Alzheimer’s disease, obtained from the UCSF Neurodegenerative Disease Brain Bank and Brazilian BioBank for Aging Studies, a special resource that was co-founded by Grinberg. The São Paulo-based biobank collects print samples from a wide population of deceased people, including many without neurological diagnosis whose brains nevertheless show signs of neurodegenerative disease at an early stage, which is very difficult to study in humans.
First, led by Kampmann lab MD / PhD student Kun Leng and PhD student Emmi Li, co-authors of the study, the team examined print from 10 donor brains using a method called single-nucle RNA sequencing, which allowed them to combine neurons based on gene activity patterns. In an area of the brain called the entorhinal cortex, one of the first areas to be attacked by Alzheimer’s, the researchers identified a specific subset of neurons that began to disappear very early in the disease. Later in the course of the disease, the researchers found, a group of similar neurons also initially died when degeneration of the frontal frontal gyrus reached the brain.
In each region, these vulnerable cells were identified by the expression of a protein called RORB. This allowed researchers at the Grinberg neuropathology laboratory, led by laboratory deputy manager Rana Eser, to study in more detail RRB-expressing neurons in brain tissue from a larger group. of 26 donors. They used histological staining techniques to study how cells were both from healthy people and from those with early and late stage Alzheimer’s. This work confirmed that neurons that express RORB actually die early in the disease and also accumulate tau tangles earlier than neighboring neurons, which do not express RORB.
“These findings support the notion that tau buildup is a critical driver of neurodegeneration, but we also know from other data from Grinberg’s laboratory that not all cells that build these collections are correct. so likely, ”said Leng, who plans to continue studying factors due to selective vulnerability of RORB neurons using CRISPR-based technology the Kampmann laboratory has developed.
It is unclear whether RORB itself causes selective cell vulnerability, the researchers said, but the protein provides a valuable new molecular “treatment” for future studies to understand what is causing it. on these cells shifting to Alzheimer’s pathology, and how their vulnerability may be reversed. .
“Our discovery of a molecular identifier for these vulnerable cells allows us to examine in detail why they are compliant with pathology, and what could be done to make them more stable,” Leng said. . “This would be a completely new and more focused way of developing treatments to prevent or prevent the spread of Alzheimer’s disease. ”
Authors: Grinberg and Kampmann are both faculty members of the Department of Neurology at the UCSF Weill Institute for Neurosciences. Additional authors of the study were Antonia Piergies, Rene Sit, Michelle Tan, Norma Neff, Song Hua Li, Alexander Ehrenberg, William W. Seeley, and Salvatore Spina of UCSF; Roberta Diehl Rodriguez, Claudia Kimie Suemoto, Renata Elaine Paraizo Leite, and Carlos A. Pasqualucci of the Universidade de São Paulo in Brasil; and Helmut Heinsen, from the Universidade de São Paulo and the University of Würzburg in Germany.
Funding: The research was supported by the US National Institutes of Health (NIH) (F30 AG066418, K08 AG052648, R56 AG057528, K24 AG053435, U54 NS100717); NDSEG alliance; Alzheimer’s Society Alliance (AARF 18-566005); Fundação de Amparo à Pesquisa do Estado de São Paulo and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (FAPESP / CAPES 2016 / 24326-0); and Chan Zuckerberg Biohub researcher award. UCSF Neurodegenerative Disease Brain Bank is supported by the NIH (AG023501, AG019724) Tau Consortium, and the Bluefield Project to treat FTD.
Publications: The authors do not cite competing interests.
The University of California, San Francisco (UCSF) focuses specifically on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate level education in the life sciences and health professions, and excellence in patient care. UCSF Health, UCSF’s premier academic medical center, comprises high-end specialist hospitals and other clinical programs, and has links throughout the Bay Area.