A research team at the University of California, Riverside School of Medicine has identified a pathway that includes astrocytes, a class of nervous system support cells, that may shed light on why seizures occur there. the subset of multiple sclerosis, or MS, patients.
Survey results, available in ASN Neuro, promote a scientific understanding of how seizures arise in MS and could form the basis for better therapies to control seizures against treatment in MS and other brain diseases.
Characterized by an episodic progressive decline in neurological activity, MS affects more than 900,000 people in the United States. This autoimmune disease damages the fatty cell – myelin – which secures zero fiber, which impedes the speed of signals in the central nervous system. Although not classically seen as a specific symptom of the disease, seizures occur three times more often in MS patients than healthy individuals and may increase symptoms. Seizure MS patients also have a lower quality of life and a higher mortality rate. The mechanisms that cause seizures in MS patients are not yet understood.
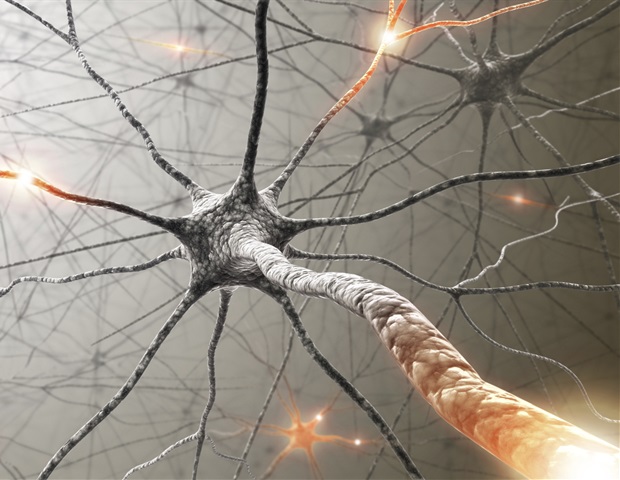
During seizures, there is a disorder between inhibition and excitation and a clump of neurons burning together out of control.
Seema Tiwari-Woodruff, Professor of Biomedical Sciences, UCR and Lead Author
Neurons are cells in the central nervous system that transmit information between the body or other neurons to allow us to move, feel, and think. Astrocytes provide the rapidly maintained environment that the neurons must accomplish by controlling the molecular signals present in the brain. Seizures can occur when astrocytes cannot keep up with this function.
Tiwari-Woodruff and her colleagues studied postmortem brain tension received from MS patients who experienced seizures (7 samples) and MS patients who did not (21 samples). The team found that astrocytes in the hippocampal samples taken from MS patients with seizures showed that they were less able to regulate the types of symptoms that were likely to cause seizures. They observed reduced synaptic glutamate (EEAT2), water-damaged and potassium ion buffer (AQP4) and altered gap-binding between astrocytes (CX43) in MS patients with seizures. In addition, links between astrocytes were altered in MS patients with seizures, a finding that has also been observed in epileptic brain but has never been seen before in MS patients.
“The most interesting aspect of the study was the discovery that astrocytes in the brain of MS patients with seizures looked very similar to astrocytes in epileptic brain,” said Andrew S. Lapato, a former graduate of the University of Colorado, Anschutz Medical Campus who as the first author did the work as part of his graduate studies in the Tiwari-Woodruff laboratory. “Researchers may be able to strengthen astrocytes’ support functions or compensate for their dose to prevent or treat seizures in MS patients.”
EAAT2 is the most widespread glutamate transporter in mammalian brains. A decrease in EAAT2 allows the neurons to burn more frequently, leading to increased capture activity. The decrease in this carrier was observed in both patients with MS and temporal lobe epilepsy.
AQP4 maintains the size of the extracellular space that allows ion movement across the connective tissue of the nervous system. A decrease in AQP4 allows for the increase of extracellular potassium ion density, which can degrade neurons and lead to hyperexcitability and long-stimulated stimulus seizures. The researchers found that these results are similar to epilepsy, suggesting a similar process in MS patients with seizures.
Previous studies have found that CX43, the major isoform connexin expressed by astrocytes, is altered in response to inflammation or demyelination. Increased CX43 sensitivity is also common in patients with epilepsy. While this study was unable to draw a more definitive link between CX43 and capture activity, it does open another avenue for study in future studies.
For this study, the team obtained 28 brain strain samples from the NeuroBioBank National Institute of Health brain bank / Human Brain & Spinal Fluid Resource Center at the University of California, Los Angeles. The samples in the study were 57% female patients and 43% male patients. The samples for MS with seizures represent almost identical male and female patients.
“One of the treasures of getting post-mortem brain tissue for our study is that we can use it to see how expressed proteins differ among others. MS patients, “Tiwari-Woodruff said.” If we don’t know what the disease looks like, we don’t know what we can do to treat it. “
Source:
University of California – Riverside
Magazine Reference:
Lapato, AS, et al. (2020) Astrocyte Glutamate uptake and aqueous Homeostasis are isolated in Hippocampus of patients with multiple sclerosis with seizures. ASN Neuro. doi.org/10.1177/1759091420979604.