Alzheimer’s Disease (AD) seems to be more diverse than our traditional models suggest.
Postmortem, an RNA sequence has revealed three main molecular subtypes of the disease, each of which manifests differently in the brain and has a specific genetic risk.
Such knowledge could help us to predict who is most vulnerable to each subspecies, how their disease might progress and what treatments would be best for them. could lead to better results.
It could also explain why finding effective treatments for AD has been so challenging to date.
Our current mouse models for pharmacokinetic study match a specific subset of AD, the authors found, but not all subtypes at once.
This may “partly explain why most drugs that have been successful with specific mouse models do not align with common human trials across all AD subtypes,” they say.
“Thus,” the authors conclude, “subtyping patients with AD is an urgent step toward a thorough cure for this devastating disease.”
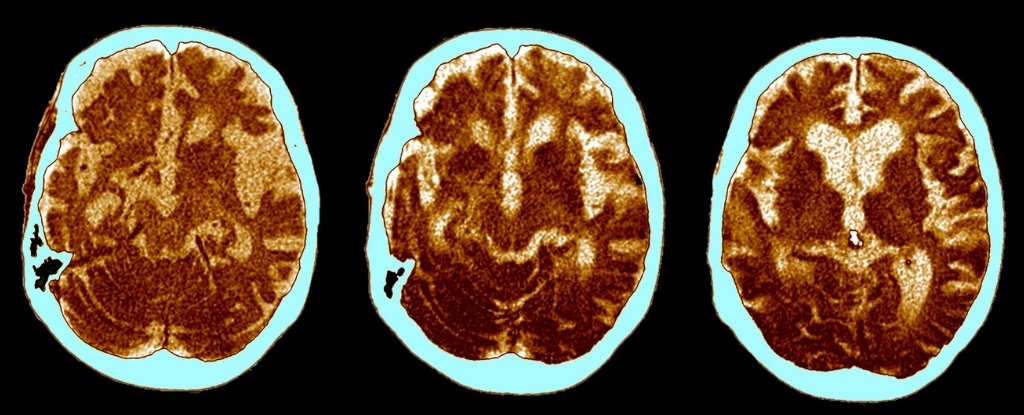
AD is traditionally thought to be characterized by clumps of amyloid-beta (Aβ) proteins, as well as clumps of tau proteins (NFTs) found in postmortem biopsies of the brain.
Both of these symptoms have been linked to the disease, but in the last few years we have been building our main ideas about what they do to our brains.
Accumulations of Aβ and NFT are generally thought to drive neuronal and synaptic loss, mainly within the cerebral cortex and hippocampus. Further degeneration then follows, including inflammation and degeneration of the immune system’s nerve cover, which causes symptoms in our brains to slow down.
Surprisingly enough, however, recent evidence has shown that up to a third of patients with clinical confirmation, postmortem biopsies do not have Aβ plaques. Moreover, many of those found with records at the time of death did not show mental impairment in their lives.
Rather than an early stimulus of AD, slowing down neurodegeneration and driving memory loss and upset, in some people, Aβ tablets appear to be latecomers.
On the other hand, recent evidence indicates that tau proteins are present from the earliest stages.
As a result of this research, it is very likely that there are specific subtypes of AD that we have not yet separated. The new research has helped with three main strands.
To do this, researchers analyzed 1,543 transcriptomes – the genetic processes expressed in the cell – across five brain regions, which were collected post mortem from two AD consortia.
Using RNA sequences to visualize these transcripts, the authors identified three main molecular subtypes of AD, which correspond to different irregular pathways.
These include: susceptibility to tau-mediated neurodegeneration; amyloid-β neuroinflammation; synaptic signaling; immune activity; organization of mitochondria; and myelination.
All subtypes were independent of age and depth of disease. Their molecular names were present in all brain regions, but especially in the hippocampus, which is largely associated with the formation of new memories.
Moreover, Aβ and tau proteins could not fully explain the various subtypes, which indicate that brain impairment is “dependent on or fully dependent on” the accumulation in the brain.
In fact, only about a third of AD cases carried these consistent signs of a ‘normal’ AD presentation. The rest of the cases showed opposite forms of gene regulation within molecules, which resulted in complex changes in several brain pathways and cell types.
“Aβ and tau accumulation are more likely to be mediators or end-effects of neurodegeneration and inflammation, independent of hippocampal loads,” the authors write.
In other words, the direct presence of Aβ and tau nuclei may not be as important as the way in which they interact with each other and other cellular processes.
Comparing the results with conventional mouse models, the authors found a significant imbalance. The majority of mouse models used in clinical research are based on ‘normal’ manifestations of AD, which would cover only a third of the cases in this study.
This means that proven treatments on mice may not work for all patients. To take a more personal approach, scientists have been trying to identify and validate molecular biomarkers just like these.
“As we have shown, AD subtypes have very different transcription signatures and therefore may require specific treatments,” the authors conclude.
“Because many subtype-specific key regulators have different directions in some AD subtypes, it is also possible that drugs that reduce AD symptoms in one subtype will produce symptoms in another subtype.”
More research is needed to confirm this hypothesis, but that is just the kind of information that we need.
The study was published in the Advances in science.