A preclinical study by the Morsani College of Medicine research team at the University of South Florida Health (USF Health) has found new tools for how Zika virus can be passed from mothers to their children during pregnancy – a process known as trans- just put.
The researchers showed, for the first time, that specific cells that line the uterus (maternal leaf cells) act as reservoirs for the spread of the trimester-dependent virus through the placenta – accounts for both the increased vulnerability of the fetus to Zika disease in the first trimester and for the more dangerous congenital defects seen early in late pregnancy. They also report that the tizoxanide agent inhibits ZIKA virus in laboratory-grown maternal stem cells, offering promise for inhibition of potentially malignant gene transmission. cause shape and brain damage in developing fetus and infants.
The results appeared December 1, 2020 in the Journal of Ornithology.
The study was led by co-lead investigators Ozlem Guzeloglu-Kayisli, PhD, associate professor of Health obstetrics and gynecology at USF, and Charles J. Lockwood, MD, senior vice president of USF Health, dean Morsani College of Medicine, and its professor of obstetrics and gynecology specializing in maternal-fetal medicine.
If we can better understand the vertical spread of Zika virus and prevent infection in maternal (deciduous) cells early in pregnancy, the virus does not pass through the placenta to reach the fetus and is less likely to be malignant. cause side effects. “
Ozlem Guzeloglu-Kayisli, Lead author of the paper
The widespread global alarm that caused the spread of the Zika virus by mosquitoes across America in 2015-2016 after the virus almost disappeared but disappeared in 2017. However, recovery is still possible in areas where the Aedes aegypti mosquito is common, and there is no treatment or vaccine available for Zika virus infection.
Although most adults with Zika infection show no symptoms, the virus can cause minor flu-like symptoms, and in rare cases it has been linked to Guillain-Barre syndrome. . However, Zika is the biggest concern for pregnant women, as up to one in 10 new mothers who are under the influence of mothers are associated with Zika, including smaller head sizes than normal (microcephaly) which can lead to developmental disabilities and other health problems. Zika has also been linked to pregnancy complications, including premature birth, preeclampsia and premature birth. Plus, time seems important. Mothers infected in the first trimester are more likely to have babies with severe Zika miscarriage than mothers infected in the third semester.
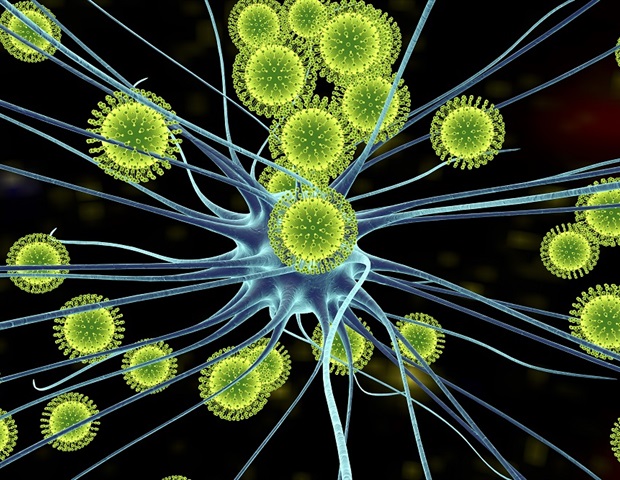
The placenta, the organ that provides maternal oxygen and nutrients to the growing fetus, has ways to prevent most pathogens, including viruses, from becoming crosses the protective barrier from mother-fetal. It is assumed that a subtype of fetally derived placental cells called syncytiotrophoblasts, in direct contact with maternal blood, is the site where the Zika virus enters the placenta, leading to infection possible fetal. However, Dr. Ozlem Guzeloglu-Kayisli said, these particular trophoblasts resist the binding and reproduction of Zika virus.
To learn more about how to get Zika through the placental wall, the USF Health team began by examining the cell and molecular mediators of Zika virus reproduction. Their key findings included the researchers:
-Show specific uterine cells from both pregnant or infertile women were highly infected with the Zika virus. These immunologically active skeletal cells, which line the uterus in preparation for and during pregnancy, make up the maternal part of the placenta closest to the fetus.
-Currently more than 10,000-fold expression of the Zika virus entry receptor in maternal leaf cells than in the fetal trophoblasts. Once inside the mother’s cells, the Zika virus (RNA virus) takes over the cell apparatus to make proteins needed to copy its genetic material and to bury new viral grains. . The proliferation of viral grains released from the maternal cells are then passed through finger-like vascular projections (villi) on the surface of the placenta where they attach to fetal trophoblast cells that are Zika virus face.
-Fun that the efficacy of viral reproduction was much greater in the first trimester decimal cells than it was in those from pregnancy.
-Confirmed maternal (decidual) cells appear to be a source for primary Zika virus infection and promote subsequent transmission through the placenta to the fetus. In addition, trimester-dependent responses of decidual cells to the Zika virus help explain why pregnant women with Zika infection and why the after-effects are worse. in the first trimester than they are at the end of the pregnancy, “the study authors wrote.
-Tisoxanide, the active metabolite of FDA-approved antiparasitic drug nitazoxanide, has currently effectively inhibited Zika virus infection in maternal decidual cells and fetal trophoblast cells. The drug has been shown to carefully inhibit a wide range of flu-like viruses and is being clinically tested for coronavirus. The finding deserves further testing on tizoxanide to prevent the viral spread of Zika virus and thus protect the fetus from harmful effects, the researchers concluded.
Source:
University of South Florida (USF Health)
Magazine Reference:
Guzeloglu-Kayisli, O., et al. (2020) Zika viral infectious detection cells undergo a gestational age – dependent sex immune response and allow Zika trophoblast: affecting direct transmission. Journal of Ornithology. doi.org/10.4049/jimmunol.2000713.