Chimney antigen receptor T-cell therapy, or CAR T, is a relatively new type of treatment approved for the treatment of several types of invasive B cell leukemias and lymphomas. Many patients have strong responses to CAR T; however, some have little response and develop disease progression rapidly. Unfortunately, it is not fully understood why these patients progress. In an article published in Proceedings of the Royal Society B., Moffitt Cancer Center researchers use mathematical modeling to help explain why CAR T cells work in some patients and not in others.
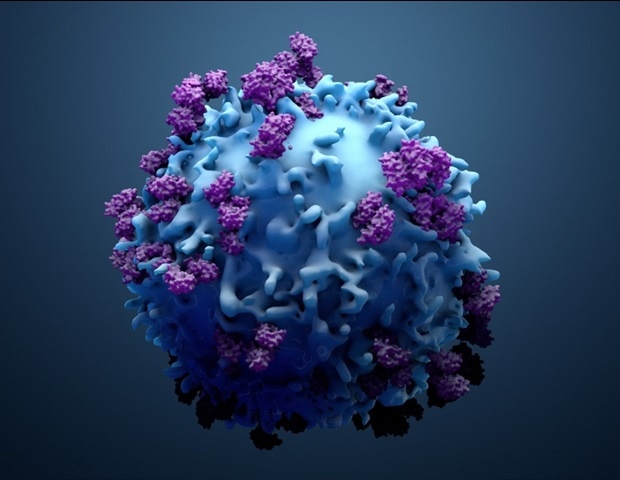
CAR T is a type of personalized immunotherapy that uses the patient’s own T cells to target cancer cells. T cells are extracted from a patient and genetically modified in a laboratory to add specific receptors that target cancer cells. The patient then undergoes lymphodepletion with chemotherapy to reduce some of their normal immune cells to aid in the proliferation of the CAR T cells that are introduced into the patient, where they have access work and attack the eardrum.
Mathematical modeling has been used to help predict how CAR T cells behave after they have been implanted in patients; however, no study has considered how interactions between the normal T cells and CAR T cells affect the dynamics of the treatment, especially as the nonlinear T cell kinetics -into the chances of medical success. Moffitt researchers combined clinical data with mathematical and statistical modeling to address these unknown factors.
The researchers prove that CAR T cells are effective because they expand rapidly after they are reintroduced to the patient; however, it has been shown that the modified T cells compete with the existing normal T cells, which may limit their ability to expand.
“Treatment success is largely dependent on the ability of CAR T cells to proliferate in the patient, and this is directly dependent on the efficacy of lymphodepletion that reduces normal T cells before CAR T is implanted,” said Frederick Locke, MD , co-lead study author and vice chair of the Department of Blood and Marrow Transplant and Cell Immunity in Moffitt.
In their model, the researchers found that tumor removal is a random, but potentially very similar, event. Despite this randomized treatment, the authors showed that differences in timing and likelihood of treatments are largely determined by variability among patient and disease factors. The model demonstrated that treatments tend to occur early, within 20 to 80 days before CAR T cell degeneration, while disease progression tends to occur over a wider time range between 200 to 500 days after treatment.
The researcher model can also be used to test new therapies or propose a revised clinical trial design. For example, the researchers used their model to show that another round of CAR T-cell therapy required second lymphodepletion chemotherapy to improve patient outcomes.
“Our model confirms the notion that adequate lymphodepletion is an important feature in determining a stable response. The development of modified CAR T cells to further proliferate and prolong life in vivo may lead to more appearance and duration of response, “explained Philipp Altrock, Ph.D. D., lead study author and assistant of the Department of Integrated Mathematical Oncology at Moffitt.
Source:
H. Lee Moffitt Cancer Center & Research Institute