A new study was published in the Journal of Alzheimer’s disease conducted by researchers at Marqués de Valdecilla University Hospital-IDIVAL, in collaboration with researchers at Bonn University Medical Center, suggests that major surgery is a promoter or accelerator of Alzheimer’s disease (AD) .
Carmen Lage was the first published author and lead researcher Pascual Sánchez-Juan.
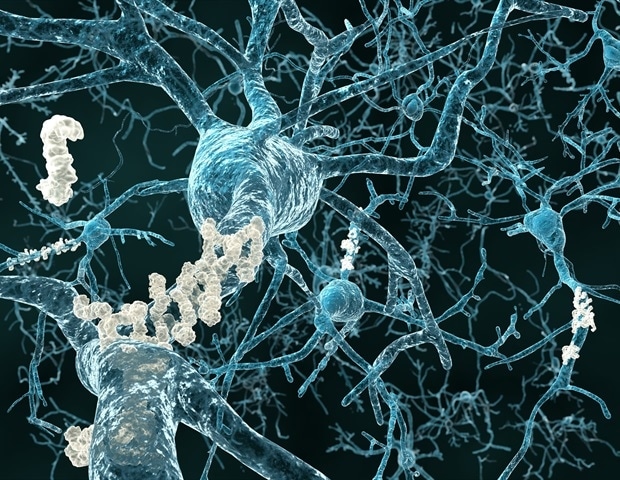
AD is one of the biggest public health challenges. From the moment the first lesions appear in the brain to the clinical manifestations, it can take up to 20 years. Today we can detect these original lesions through biochemical markers such as amyloid-β, which is one of the major proteins accumulated in the brains of Alzheimer’s patients.
The frequency of amyloid-β deposits in healthy people increases with age, and after the age of 65, they would be present in up to a third of the population. However, it is not known what determines how the disease progresses largely to depression or even in inactive behaviors.
Although experience of postpartum depression has been experienced for a long time, there are few studies linking it to AD. In the clinic, the patient ‘s relatives often tell us that a memory problem started after surgery or hospital admission. This begs the question: Is this just memory bias or has surgery stimulated the appearance of symptoms in previously affected brains? “
Carmen Lage, First Author Study, Marqués de Valdecilla-IDIVAL University Hospital
This is the question that prompted the work developed by researchers from the Marqués University Hospital of Valdecilla-IDIVAL examining the link between cerebrospinal fluid amyloid-β (CSF) levels and surgery.
The researchers gave mental tests to healthy people over 65 years before undergoing orthopedic surgery; they received samples of CSF to determine amyloid-β levels during anesthesia, and then administered the same tests again nine months later.
The main result was that half of the patients’ psychosis worsened compared to their preoperative state, and those who had amyloid-β levels changed a similar pattern. early AD, in which memory problems appeared.
Carmen Lage said: “Prior to surgery, memory test scores of subjects with abnormal amyloid-β levels were different from scores of subjects with normal levels, but nevertheless after surgery, they were fine. These results lead us to conclude that major surgery can induce different patterns of cognitive changes, depending on whether or not Alzheimer’s pathology changes before.While subjects without amyloid-β pathology showed a decline that does not affect memory, perhaps related to factors inherent in the surgery itself, those with amyloid-β pathology suffered from a cognitive decline that mainly affected memory, and was consistent with the first clinical manifestations of AD and therefore associated with greater likelihood of progression to depression. “
Dr Pascual Sanchez-Juan said: “The progressive growth of our society and the development of surgical techniques mean that more and more older and frail people are having surgery. Pre-surgery assessment is always assessment of the viability of the card or respiratory operation, however, the potential impact of the operation on the patient’s brain is not usually determined.Our results would claim that preoperative assessment studies include psychiatric tests, and even analysis of Alzheimer ‘s biomarkers, especially once these are widely available in plasma. “
Source:
Magazine Reference:
Lage, C., et al. (2021) Major surgery affects memory in individuals with Amyloid-β cerebral pathology. Journal of Alzheimer’s disease. doi.org/10.3233/JAD-191229.