The side effects of a drug, or the effects of treatment such as chemotherapy, do not just depend on your body. The success of a particular medicine also depends on the trillions of bacteria in your gut.
The 100 trillion bacteria that live within the human digestive tract – known as the human gut midge – help us remove nutrients from food, boost the immune response and changing the effects of drugs.
Recent research, myself included, has affected gut microorganisms in seemingly unrelated states, from responding to cancer treatments to obesity and a number of brain diseases, including Alzheimer’s , Parkinson’s disease, depression, schizophrenia and autism.
Underlying these individual observations seems to be the unifying notion that the gut microbiota transmits signals to the gut and that these symptoms have far-reaching effects on a wide range of gut. target figs.
I am a medical oncologist and my research includes the development of novel treatments for melanoma. To assess whether microbome modification could benefit cancer patients, my colleagues and I evaluated the transition of fecal matter from melanoma patients who responded well to immunotherapy to those patients who failed immunotherapy.
Just published in the magazine Science, our results indicate that this treatment helped reduce tumors of advanced melanoma patients when other treatments had not worked.
What binds cancer and gut bacteria?
Gut microbiota has been linked to the success and failure of multiple cancer treatments, including chemotherapy and cancer immunotherapy with immune checkers such as nivolumab and pembrolizumab.
In the most recent studies, the sex and relative numbers of gut bacteria determined the likelihood that a cancer patient would respond to drugs called “immune checkers.”
This research showed that differences in the gut microbiome between individual patients were associated with different outcomes for these drugs. But it is not certain what exact mechanisms underlie microbiome-protective interactions.
Can fecal microbes help drugs to treat melanoma severely?
Oncologists often treat patients with advanced melanoma using immunotherapies that target specific proteins on the surface of immune cells called PD-1 and CTLA-4. These work in a subset of patients, however – 50-70 percent of patients have cancers despite treatment.
No medical treatments were agreed for melanoma patients who failed with PD-1 immunotherapies.
To investigate whether some microbes could increase the effectiveness of PD-1 immunotherapies, my colleagues and I developed a study in which we collected fecal microbes from patients who had responded well to this treatment and donated them to cancer patients who did not benefit. from the checkpoint drugs.
We chose stool from patients who responded well to the hunt-based immunotherapy to have more bacteria involved in helping reduce the cancer.
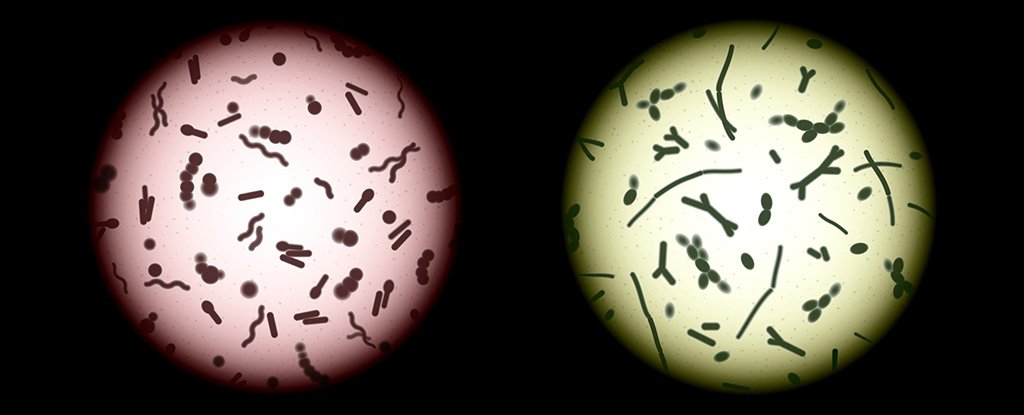
 (Diwakar Davar / CC BY-ND)
(Diwakar Davar / CC BY-ND)
Since it is difficult to identify one or two species of bacteria that are responsible for a beneficial response to these treatments, we used the entire bacterial community – hence fecal microbe transmission.
Transplant recipients were patients who had never responded to melanoma with immunotherapy. Both recipients and donors were screened for diseases to ensure that no infectious agents were transmitted during transplantation.
Following a biopsy of their tumor, patients received fecal microbe transfusion from patients who benefited from immunotherapy in combination with a drug called pembrolizumab, which was held every three weeks.
My colleagues and I evaluated fecal microbe transplantation 12 weeks after treatment. Patients whose cancers had shrunk or remained the same size after fecal microbe transfusion were given pembrolizumab for up to two years.
Novel clinical trial results
 (Diwakar Davar / CC BY-ND)
(Diwakar Davar / CC BY-ND)
After this fecal microbe transfusion treatment, six out of 15 patients in the previous or previous study had tumors. The treatment was well received, although some patients experienced minor side effects including muscle weakness.
When we analyzed the gut microbiota of treated patients, we found that the six patients whose cancers had settled or improved showed greater numbers of bacteria that had previously been associated with responses to immunotherapy.
My colleagues and I also analyzed blood and tumors from respondents. In doing so, we found that the responders had lower levels of malignant immune cells called myeloid cells, and higher levels of memory immune cells. Furthermore, by analyzing proteins in the blood serum of treated patients, we observed decreases in levels of key immune system molecules associated with resistance to responders.
These findings suggest that the introduction of intestinal microorganisms into a patient’s colon may help the patient respond to drugs that increase the ability of the immune system to recognize and tumor cells.
Ultimately we hope to move beyond microbial fecal transplants to specific accumulations of microbes in cancers other than melanoma, paving the way for conventional microbe-based drug treatment to treat immunotherapy-resistant tumors. to handle. ![]()
Diwakar Davar, Associate Professor of Medicine, University of Pittsburgh.
This article is republished from The Conversation under a Creative Commons license. Read the original article.