When patients with COVID-19 arrive in emergency rooms, there are few ways for doctors to predict which ones are more likely to be seriously ill and require intensive care and which ones are more likely to receive back quickly.
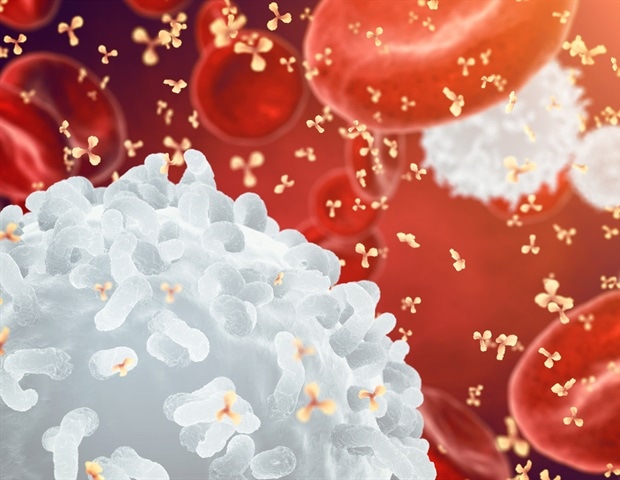
Yale’s new research could help them identify important early things. In a recent study, researchers report that a series of biomarkers, or biological markers, associated with white blood cell activity and obesity may predict severe outcomes in COVID-19 patients.
The findings are reflected in the Feb. 26 edition of Blood clots.
“Patients with high levels of these symptoms were significantly more likely to seek care in the intensive care unit, require ventilation, or die because of their COVID-19,” said Dr. Hyung Chun, principal author, associate professor of medicine in cardiovascular medicine and pathology and director of translational studies at the Yale Pulmonary Vulnerable Disease Program.
Previously, there had been a few laboratory studies of possible symptoms of COVID-19 deficiency, including D-dimer levels, measured blood coagulation, and levels of proteins called cytokines, which are released as part of inflammatory responses in the body. However, to date, laboratory markers have not been able to predict which patients with COVID-19 became severely ill before showing clinical signs and symptoms of malignancy.
For the new study, Yale researchers used proteomic profiles – a screen for intracellular multiple proteins – to analyze samples taken from 100 patients who would go on to gain experience. on different levels of COVID-19 intensity. In all cases, the blood samples were collected on the first day of patients. The researchers also analyzed clinical data for more than 3,000 additional patients with COVID-19 within the Yale New Haven Hospital system.
They found that five proteins (resistin, lipocalin-2, HGF, IL-8, and G-CSF) associated with neutrophils, a type of white blood cell, were elevated in COVID-19 patients. who became seriously ill. Many of these proteins had previously been linked to obesity but were not associated with COVID-19 or other viral infections.
In particular, the neutrophil-enhanced biomarkers for patients who were going to experience worsening symptoms were visible before these symptoms appeared. All COVID-19 patients admitted or transferred to the ICU had elevated neutrophil activity signals, while these biomarkers remained low for patients who had never developed severe disease. None of the patients died with lower neutrophil biomarker levels.
“This is one of the first demonstrations that a set of biomarkers in the blood of COVID patients can predict the introduction of ICU, even before such patients become ill,” said study author Dr. Alfred Lee. professor of medicine in hematology, director. of the Yale Oncology-Hematology Medical Fellowship Program, and a member of the Yale Cancer Center.
Early knowledge of these symptoms could significantly improve patient treatment, the researchers said.
If there is an audit test [for these biomarkers] may be prescribed early, may give us a better sense of who is more likely to become ill and benefit from a higher level of care and consideration for treatments that affect the patient. the immune system early in their hospitalization. Many of these drugs have potential side effects, and these trials may help identify those patients who would benefit most. “
Dr. Hyung Chun, Lead Author
The study also highlights the link between COVID-19 and obesity, researchers said. The Centers for Disease Control and Prevention notes that obesity and high obesity increase the risk of serious illness from COVID-19. Obesity triples hospitalization risk from COVID-19, and body index levels have been found to be associated with risk of death from COVID-19.
Neutrophils are inflammatory cells, Lee said, so it makes sense that they would be elevated in the context of both obesity – which includes chronic, low-grade inflammation – and COVID-19 , which causes hyperinflation in the most severe cases, leading to thin tissue and organ failure.
“There are also indications that neutrophils may be involved in thrombosis or hemorrhage,” said Lee, another troubling symptom of COVID-19.
The researchers will expand their study of the link between biomarkers and COVID-19 by looking at patients who have recovered from a real illness.
“We hope these decisions will encourage other organizations to look at their own patient numbers,” Chun said, adding that they need additional diagnostic studies to support improvement. diagnostic tests for these biomarkers.
The research involved colleagues from across many different Yale departments, including Matthew L. Meizlish, MD-Ph.D. student; Dr. Alex Pine, professor of medicine in hematology and staff physician at VA Medical Center in West Haven; Jason Bishai, graduate student; Hanming Zhang and C-Hong Chang, postdoctoral relatives; and Dr. David van Djik, professor of medicine in epistemology.
“The evolution of our decisions certainly demonstrates the power of collaboration, which has emerged as one promising part of this pandemic that we will continue to use for the benefit of patients,” Lee said.