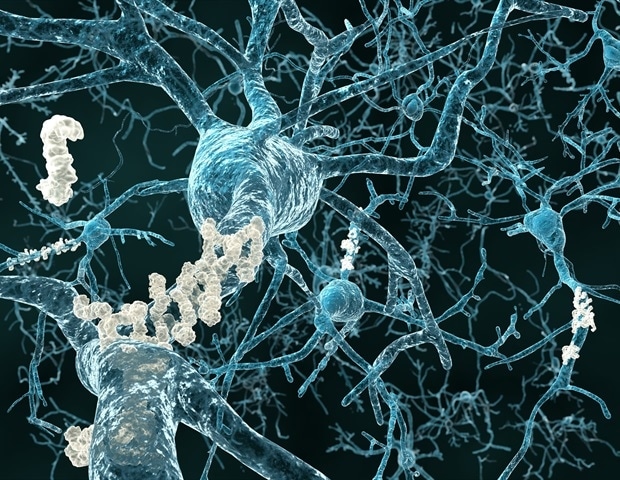
Amyloid-beta and tau are the two main anabolic protein deposits that accumulate in the brain during the development of Alzheimer’s disease, and if they detect the buildup at an early stage clinicians can intervene before the condition gets caught. A team led by researchers at Massachusetts General Hospital (MGH) has now developed an automated method that can identify and detect the development of harmful tau deposits in a patient ‘s brain. The research, which is published in Science Translational Medicine, that could lead to earlier studies of Alzheimer’s disease.
Although our understanding of Alzheimer’s disease has grown significantly in recent years, many attempts to treat the condition so far have failed, possibly because medical interventions have taken place after the rate at which brain damage becomes irreversible. “
Justin Sanchez, Lead Author, Data Analyst, Gordon Center for Medical Imaging at MGH
In an effort to develop a method for earlier diagnosis, Sanchez and his colleagues, led by Keith A. Johnson, MD, of the Radiology and Neurology departments at MGH, evaluated brain images of amyloid-beta and tau obtained with the spread of positron tomography, or PET, in 443 adults participating in several observational studies of age and Alzheimer’s disease. Participants spanned a wide range of ages, with varying levels of amyloid-beta and brain impairment – from healthy 20-year-olds to elderly patients with a clinical diagnosis of Alzheimer’s dementia. The researchers used an automated method to identify the most vulnerable brain region in terms of cortical tau buildup in each individual PET scan.
“We thought that using our method on PET imaging would allow us to detect the original accumulation of tau cortical in normal and intelligent people, and monitor the distribution of tau from this original location to regions. other brains in connection with amyloid-beta deposition and the brain weakening of Alzheimer’s disease, “Sanchez explains. He notes that it appears to be cortical tau, when it spreads from its original site to brain regions. neocortical under the influence of amyloid-beta, the “bullet” that damages brains in Alzheimer’s disease.
The approach revealed that tau deposits first appear in the rhinal cortex region of the brain, independently of amyloid-beta deposits, before spreading to the nearby temporal neocortex. “We observed primary cortical tau accumulation at this initiation site in normal individuals with no evidence of elevated amyloid-beta, as early as 58 years of age,” Sanchez said.
Importantly, when the scientists followed 104 participants for two years, they found that people with the highest initial levels of tau at the starting point exhibited the greatest spread. of tau throughout the brain over time.
The findings show that PET doses of tau that specifically target specific brain regions may predict an individual’s risk of future tau accumulation and Alzheimer’s disease as a result. Focusing on tau when detected at an early stage could halt the situation or delay progress.
“Clinical trials evaluating the efficacy of anti-tau therapeutic therapy would benefit from an automated, individual imaging approach to select normal individuals who are vulnerable to future tau transmission, and as that furthers our efforts to provide effective interventions to patients at risk for Alzheimer ‘s disease, “said Sanchez.
Source:
Massachusetts General Hospital
Magazine Reference:
Sanchez, JS, et al. (2021) Cortical origin and initial distribution of medial temporal tauopathy in Alzheimer’s disease were assessed by positron diffusion tomography. Science Translational Medicine. doi.org/10.1126/scitranslmed.abc0655.