A new three-drug, oral, six-month treatment is giving hope to patients in Tajikistan with major drug-resistant forms, who so far had few treatment options and poor prognosis.
Tajikistan is the first country in Central Asia and the second in the world after Ukraine to provide access to the novel ‘BPaL’ regimen for patients suffering from widespread drug-resistant tuberculosis (XDR-TB) under operating research conditions from December 2020. The regimen contains three drugs –bedaquiline, pretomanid and linezolid.
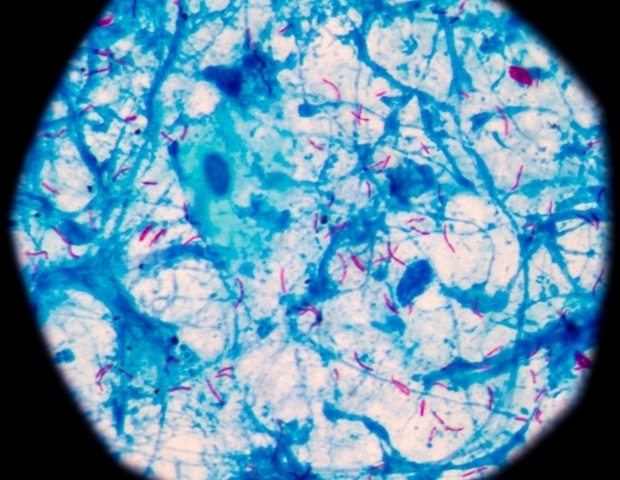
XDR-TB is caused by bacteria that are resistant to some of the most effective anti-TB drugs and these rays develop from misdiagnosed treatment of patients with multidrug-resistant TB (MDR-TB).
“The BPaL regimen offers the shortest possible course of treatment for XDR-TB patients, without injectable drugs, is easy to use and more accessible,” says Veriko Mirtskhulava, senior epidemiologist at KNCV Tuberculosis Foundation, NGO internationally dedicated to the eradication of TB.
“The standard treatment schedule for patients with XDR-TB includes 7-8 antibiotics for at least 18 months, including none of the injectable drugs, which not all patients can tolerate. . “
The BPaL regiment, developed by the non-profit organization TB Alliance, is implemented in Tajikistan by the National Tube Program with support from the KNCV Tuberculosis Foundation.
“As the regimen remains a new treatment against TB, it is essential to closely monitor the feasibility, appropriateness, safety and efficacy, and ensure systematic and routine data collection,” Mirtskhulava explains. SciDev.Net.
“Tajikistan has the human resource and infrastructure capability for it. After examining the operational research data on the safety and effectiveness of the regimen, a decision will be made on scaling BPaL treatment under service delivery conditions. regular health. “
While it is possible to prevent TB and treat most with early detection and proper treatment, conventional drugs will not work in drug-resistant strains of TB. MDR-TB resists the two most potent first-line TB drugs – isoniazid and rifampicin. In addition, XDR-TB is against second-line TB drugs – any fluoroquinolone and any of the three injectable drugs – amikacin, capreomycin and kanamycin.
According to the World Health Organization, there was a ten percent increase in MDR-TB in 2019 compared to the previous year, and the worldwide cure rate of XDR-TB is only 43 percent. However, the BPaL regiment has shown success in treating 90 percent of XDR-TB patients in the Nix-TB Alliance Alliance test, which was conducted at three sites in South Africa. The results were published in the New England Journal of Medicine Last year.
“We now have initial evidence that, with the right drugs and drug regulations, TB-resistant strains could be treated with the same number of drugs and at the same time as those required for TB-sensitive treatment. drugs, ”said Sandeep Juneja, TB Alliance chief vice president of market access.
The BPaL regiment was first approved in August 2019 in the USA and recommended by the WHO under the terms of operational research. It is expected that many more countries will soon embark on operational research involving South Africa and Nigeria, as well as through efforts such as the TB Alliance’s LIFT-TB program, which is supported. from South Korea, registering patients in Indonesia, Kyrgyzstan, Myanmar, the Philippines, Uzbekistan and Vietnam.
“Our priority is to enable the rapid roll-out of BPaL regimen quickly to those in need, wherever they live. For countries where pretomanid is not yet agreed, our global trading partner Viatris has announced a patient outreach program, “Juneja explains SciDev.Net.
All three drugs in the regiment are available to approximately 150 low- and middle-income countries through the Global Stop TB Partnership Drug Facility at a cost of under US $ 1,000 per six-month treatment course.
“The agreement of this regiment [under operational researchconditions] is a major step forward for people affected by XDR-TB. However, there is an urgent need to increase the size of laboratory capacity to test against these new drugs. A recent small study from South Africa has found worrying levels of resistance to bedaquiline in rifampicin-resistant TB, ”said Khai Lin Huang, an infectious diseases physician at the Burnet Institute Melbourne, Australia.
Khai Lin explainsSciDev.Netthat combats against non – chemical substances will almost certainly occur with increased use, but the risk and impact can be managed with appropriate systems in place.
“Currently, the evidence for BPaL regimen comes from a single trial in one country, but more knowledge and data are needed. It is important that countries have a framework and capacity to be able to conduct operational monitoring and change quickly, “he added.
Ending TB disease by 2030 is among the health goals of the UN Sustainable Development Goals. Globally, 1.4 million people died and around ten million people, including 1.2 million children, were ill with TB in 2019. Eight countries accounted for two-thirds of the total new cases, with the -India manages the census, followed by Indonesia, China and the Philippines, Pakistan, Nigeria, Bangladesh and South Africa, according to WHO.