.jpg)
Even with the outbreak of pandemic coronavirus 2019 (COVID-19) pandemic, caused by the true acute coronavirus 2 (SARS-CoV-2) respiratory syndrome, new changes have emerged with increased infectivity on violence. This raises the risk of a protective escape mediated by the range of leaks in these new variables.
These include the B.1.1.7 variant SARS-CoV-2, with a typical N501Y mutation. A new introduction to the bioRxiv * server reports the effect of this bud on CD4 T cell responses, including antigen presentation on cells expressing Class II Major Histocompatibility Complex (MHC) molecules.
As soon as population immunity
The pandemic has already claimed over 2.2 million lives in just over a year. This death toll has risen from more than one hundred million reported diseases worldwide.
Despite intensive testing for new and reconstructed antivirals, the prevention and treatment of the disease has not been successful. The main push continues for non-therapeutic interventions, including wearing masks, facial and hand hygiene, and social distance, with locks being used in situations where case levels show a sudden increase.
The definitive way into herd immunity is with both a natural infection and a vaccine. The immune response is characterized by seroconversion within seven days of infection. Stable immunoglobulin G (IgG) antibodies are detected in the patient, lasting for 2-3 months at stable levels before they are excreted. Several studies have shown that immunity drops dramatically by six months after infection.
More than 70% of COVID-19 convalescent patients with CD4 T cells are reactive to SARS-CoV-2; their activity is directly proportional to specific IgG antibody titers. However, these cells are also reactive to the virus in 40-60% of uninfected individuals, indicating that the “common cold” seasonal coronaviruses activate a subset of CD4 T cells that react to the virus. later recognizes the common antigens on SARS-CoV-2.
UK variability increase
The UK variant known as the SARS-CoV-2 virus, B.1.1.7, was first reported following a genome sequencing study in December 2020. Since then, the strain has been identified in more on 50 countries. This variation has been shown to be more contagious than the parent weight by 50%, causing it to create a large and growing proportion of new cases in many areas.
In fact, the U.S. Centers for Disease Prevention and Control (CDC) predicts that the B.1.1.7 variant will gain control of series circulating globally by March 2021.
Mutation and infectivity N501Y
The standard N501Y mutation replaces asparagine for tyrosine at this position in the receptor binding domain (RBD) of viral spike protein S1 substrate. The RBD is the region that communicates directly with the host cell receptor, an enzyme 2 that converts angiotensin (ACE2).
This mutation is common to many other species, from South Africa, Brazil, Australia, Japan, Denmark, the Netherlands, and U.S. states such as Texas, Illinois, Louisiana, and Ohio. The presence of mutations at this residue appears to promote a connection between the spike and ACE2, and the better connection at this site may explain the rapid increase to the surface of this type. .
N501Y and protective deviation
However, there is a bigger question on the minds of many; does this mutation also cause or contribute to immune escape?
For one thing, N501 residue is part of the RBD epitope that is a primary target of many neutralizing antibodies isolated from COVID-19 convalescents. As a result, the wild-type RBD may have acquired antibodies that do not bind with similar efficacy to the RBD mutant.
In fact, a mouse study showed increased susceptibility and violence to the mutant snoring. The presence of some other specific mutations such as E484K may contribute to the effect of N501Y mutation on these features of the virus.
MHC-II centralized antigen presentation
Another explanation is that the mutation affects an altered immune response, which involves B and T cells. The MHC system coordinates the key molecules in this complex dance of immune cells and antigens. This system consists of molecules on the surface of cells that bind directly to antigen peptides of a specific type, according to the MHC class.
When the antigen complexes with the MHC, specific circulating T cells recognize it and expand their clone with proliferation. These T cells are capable of directly destroying the virus.
Also, the MHC-linked antigens activate CD4 T cells which in turn activate those B cells that are able to specifically identify the antigen and generate a flood of anti-SARS-CoV- antibodies. 2. These antibodies target the viral antigens and antigen fragments that are expressed on antigen-expressing cells and on the infecting cells themselves.
Disorder of TB cell coordination
This orchestrated response of B and T cells is required to elicit a strong immune response, possibly by favoring pairs of preferred pairs of B and T cell epitopes, or antibody binding sites.
The researchers in the current study aimed to investigate the effect of substitution in the amino acids found around B cell epitopes at the area where the RBD communicates with the ACE2 receptor because these were required. binding of MHC-II molecules as well, to induce TB co-occurrence.
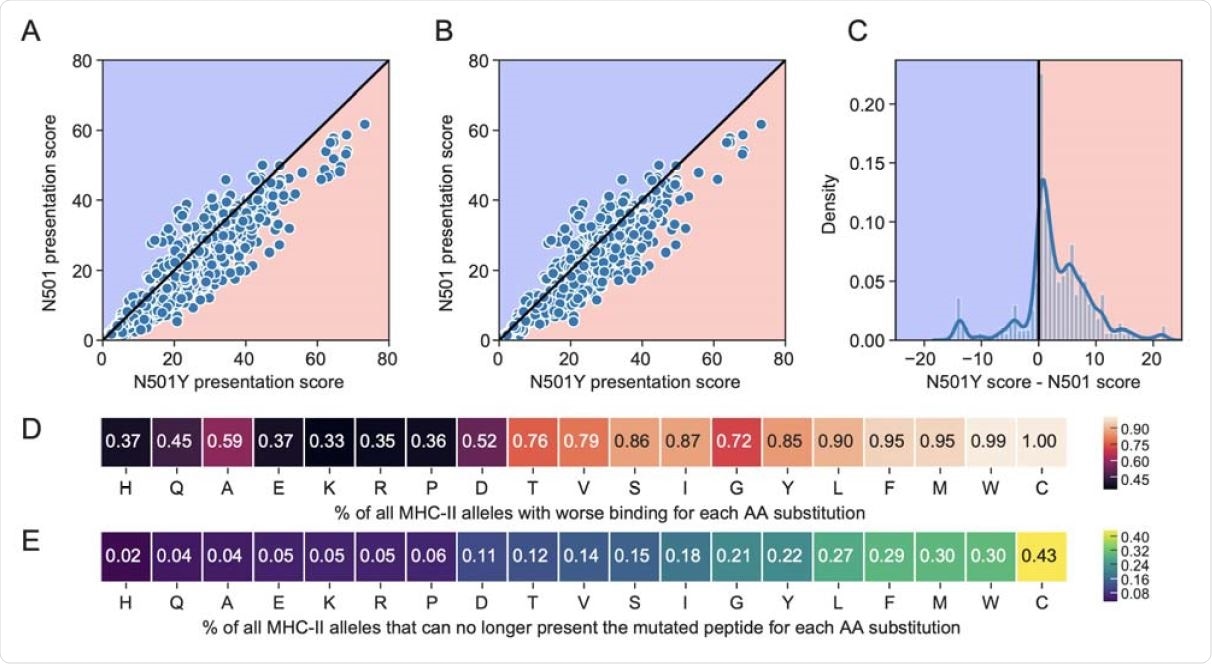
They used computer modeling to predict the antigen display uses for all 15 peptides detected at position 501, in complex with MHC-II. Comparing the calculated display scores, they found that mutant N501Y has less binding affinity for 85% of MHC-II alleles and 83% of the most common MHC-II alleles, compared to parent peptide.
Not only that, but 22% of the common alleles and alleles cannot express the mutant peptide for further activation of T and B cells.
What is the impact?
These findings suggest, at least, the potential for lower MHC-II-mediated antigen presentation with the SARS-CoV-2 virus due to the lower affinity for MHC-II molecules at this site. . Thus N501Y mutation could induce faster release of these changes with its favorable effect on spike-ACE2 binding and its unfavorable effect on MHC-II binding for most alleles .
The weakening resulting from TB cell interaction could adversely affect the production of neutralizing anti-RBD antibodies.
“The new virus variants with the critical simulation N501Y may pose a challenge to the quality of the adaptive response required for protection.. ”
This is quite possible as it relates to natural immunity as well as would be expected from conventional vaccines. Future research needs to focus on demonstrating the neutralization potential of natural disease-induced antibodies or the vaccines used to identify and neutralize these new variants with N501Y mutation.
The effect of this bud on the binding strength and specificity of neutral antibodies also needs to be studied. And finally, if the CD4 T cells activated by contact with vaccine antigens in which the wild-type spike tends to secrete antibodies to the same antigenic sequence, the introduction of the original remains of the N501 is likely to be a protective escape from the new variants.
* Important message
bioRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.