A recent study in the US, currently available on medRxiv * preprint server, supports a beneficial rather than immunopathologic role for influencing T-cells during severe infections with acute respiratory coronavirus syndrome 2 (SARS-CoV-2) – and provides several important insights for our battle against coronavirus disease 2019 (COVID-19).
The chronic and contagious pandemic COVID-19, caused by the beta-coronavirus SARS-CoV-2, has shaken the world’s healthcare systems and economy and claimed more than 2.22 million lives a year after his appearance.
The human immune system includes cellular (T cell) and humoral (B cell) immunity and plays a vital role in our defense against SARS-CoV-2. And while coordinated interaction between the cellular and humoral arms appears to be essential for effective control, T cells appear to be able to resolve the disease when B cell responses are deficient.
We know that a common feature of COVID-19 deficiency is T cell lymphopenia (i.e., reduced level of lymphocytes in the blood), which is unlikely to directly indicate T cell uptake in the infected lungs.
T cells as ‘the most valuable players’?
T cells appear to significantly increase the immunity of SARS-CoV-2; however, little is known about the phenotypic properties of SARS-CoV-2-specific T cells associated with recovery from COVID-19 malignancy. That said, some more recent studies have analyzed the characteristics of T cells recognizing SARS-CoV-2 epitopes.
Assuming that those antigen-specific cells can directly identify oral infectious cells and generate specific antibodies, they have the greatest potential to show a beneficial effect on disease recovery. They are also key targets of vaccination efforts.
In this study, a research group led by Dr. Jason Neidleman of the Gladstone Institutes and the University of California at San Francisco (USA) aims to explain the characteristics of T cells from individuals who were hospitalized in the ICU because of COVID-19 – including some who got over that successfully and some succeeded with the disease.
Deep phenotyping approach
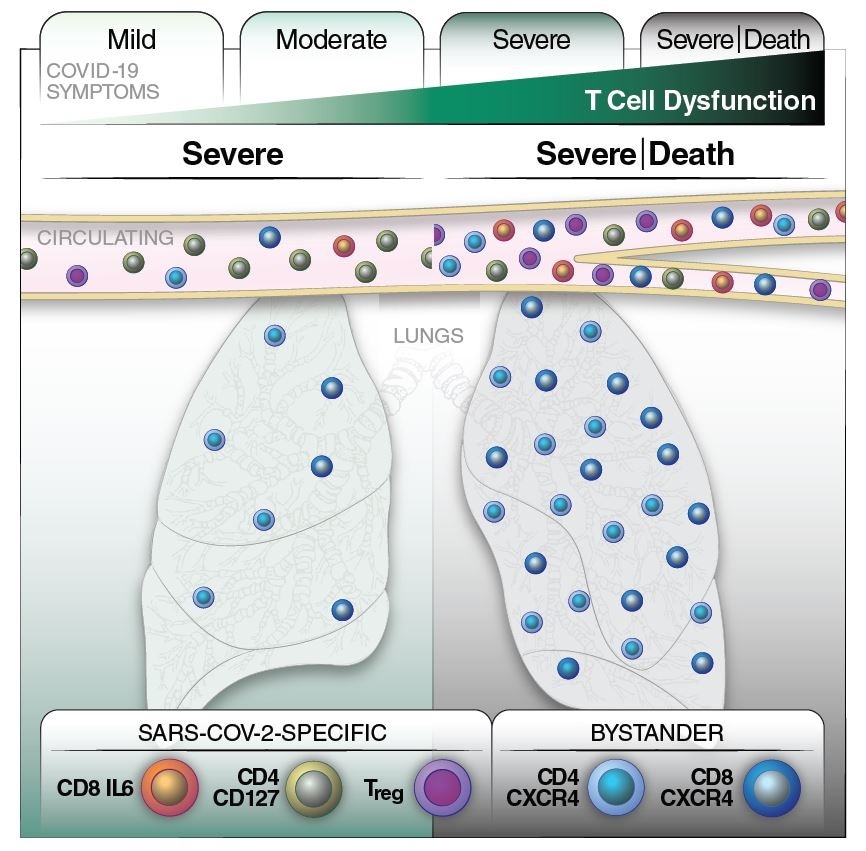
In this study, the researchers have compared whole T cells and CoV-2-specific SARS in mild, moderate, and severe cases of COVID-19. Furthermore, within the hard cases, long-term samples were analyzed in depth to identify any predictive features related to survival.
A total of 48 blood samples from 34 people infected with SARS-CoV-2 were examined, along with samples from 11 unprotected controls. Samples were taken from ICU patients classified as “true cases” (68.8%), and from hospital patients not requiring the ICU, classified as “moderate cases” (31.2%).
The scientists implemented in-depth phenotyping of whole T cells and SARS-CoV-2-specific using CyTOF 38-parameter – a recently introduced method for identifying T characters from human individuals. -leth.
This allowed the identification of specific phenotypic properties of viral T-specific bystander and associated T bystander to overcome malignancy, which was then paired with a comprehensive study of T cell characteristics present in the lungs of COVID patients. -19.
Role of SARS-CoV-2-specific T cells
In contrast to deceased patients, individuals in this study who recovered from malignant forms of COVID-19 produced high numbers of SARS-CoV-2-specific T cells capable of a physical response called homeostatic proliferation. protection.
In particular, the researchers observed an increased number of CD8-expressing transition memory T cells in patients with mild symptoms and a higher number of activated, PD1-expressing T cells in patients with true symptoms.
On the other hand, in lethal cases of COVID-19, there was a high number of SARS-CoV-2-specific regulatory T cells and a time-dependent increase in CXCR4 + T-activated cells (the latter subset of cells considered “extrafollicular” helper T cells).
When all the results are taken into account, this study represents a model in which lung-secreted T cells activated by bystander effect contribute to immunopathology, whereas SARS T cell response Non-suppressive and potent -CoV-2-specific controls pathogenesis and promotes recovery. from COVID-19 injury.
Effects for vaccination efforts
In summary, the findings of this study support a favorable rather than immunopathologic role for SARS-CoV-2-specific T T cells during acute infectious disease, along with stimulating recovery from COVID- 19.
“Taking into account the longevity of SARS-CoV-2-specific T cells, our findings suggest that strategies to enhance the efficient actions of SARS-CoV-2-specific T cells, including vaccine, beneficial for reducing COVID-19 mortality and helping to end this pandemic “, say these authors medRxiv study.
In any case, since this study was correlative and phenotypical in nature, ongoing action assessments will be required to establish any causal effect, as well as studies of larger groups of people with disease.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical practice / behavior, or be treated as information established.