Many cases have been reported where people vaccinated with coronary respiratory tract syndrome 2 (SARS-CoV-2) infection have kept the virus for longer than normal. New introduction published on the medRxiv * a server describing a patient with the 2019 coronavirus infection vaccine (COVID-19) who kept the virus at bay for an astonishing 154 days. During this time, the virus has undergone many mutations.

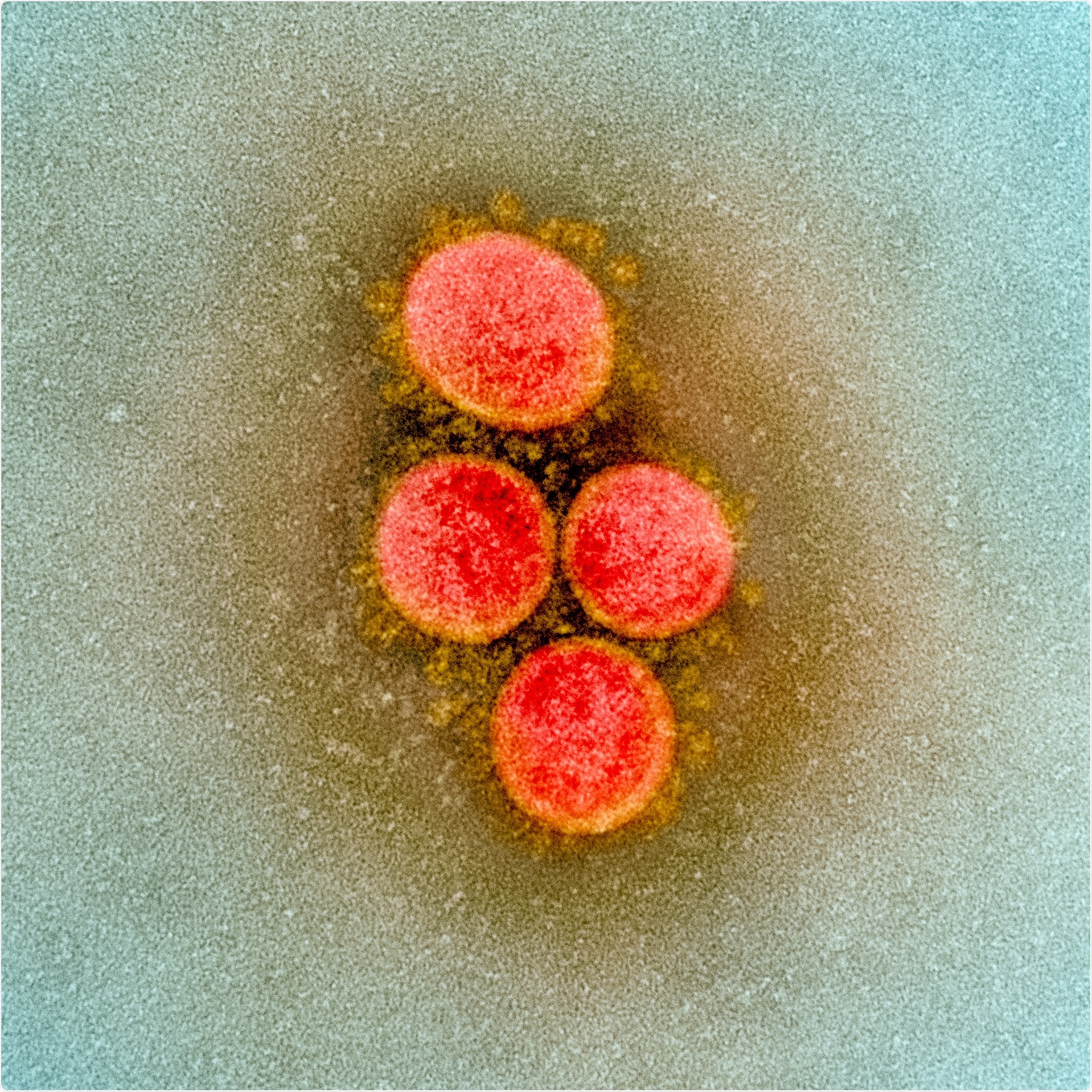
Study: Several mutations of SARS-CoV-2 appeared in a host host. Image credit: NIAID
After nearly a year of COVID-19, the virus appeared as a new variant, now known as the British variant. It is thought that this difference could lead to higher susceptibility and therefore more transmission. Following this discrepancy, which occurred almost immediately, allowed for a more in-depth study of how the mutations affected the structure of various viral proteins and the molecular determinants of disease spread. Genetic diversity is thought to arise within a host unless the virus is under selective pressure by the host immune response or by therapeutic antibodies.
The current study describes one such patient. The person was infected for over 134 days and eventually died from the disease. Throughout the course of the disease, replica virus was present in the respiratory tract. The virus also passed through several strains, compared with two other patients with low B cell counts and most other individuals with SARS-CoV-2 infection.
The patient was a woman in her seventies who was admitted to the hospital with COVID-19 infection, and severe respiratory distress syndrome (ARDS). The symptoms had been present and worsening for two weeks before admission. It was placed on high-flow oxygen and subsequently mechanically ventilated. She remained in the intensive care unit until her death, five months after admission.
The patient had a history of follicular lymphoma and had received three cycles of chemotherapy, in addition to the anti-CD20 antibody obinituzumab, which degrades B cells. This treatment was stopped just a month before she continued at the hospital. The patient was treated with steroids and convalescent plasma (CP), but not with remdesivir because she also had renal failure.
In the samples from the upper and lower clinical respiratory tract there was a live replica virus, with low threshold values (Ct) of reverse transcriptase-polymerase chain reaction (RT PCR), and high viral loads, until its death. on 156 days since confirmed. The first sample collected was held on day 20, which the researchers term day 0.
The genome sequence from this patient, as well as two other B-cell lymphoma patients were treated in the same unit at the same time, and both had severe COVID-19 over a long period of time, and also developed ARDS . The last two patients recovered completely.
The five mutations that defined this patient’s strain include D614G, 3037, 14408, and 241, along with deletion at position 28881 of the nucleocapsid antigen. Other specific mutations found in this patient include one seen only in southern Germany between March 16 and May 11, 2020. In comparison, both did not have a replica virus. another patient only for three weeks, at most, with only one or two mutations in 19 days. This depends on the expected number of mutations in this virus. In fact, the index patient had the same number of seizures for the first 21 days.
The similarity in number and pattern of mutations indicates that all three patients were infected from the same source. Visible mutations decreased by day 30, after two doses of CP, but five new mutations were established during this time and continued until day 134. Thus, a further 11 mutations occurred.
The average patient developed 16 mutations. Typically, SARS-CoV-2 viruses show 1-2 mutations per month or about 24,000 mutations per genome per year. In the 134 days, the patient’s viral genomic samples were analyzed, the expected number of mutations would be 8.6, but instead, there was an abnormal number of unidentified mutations, more than three times the number of mutations. number of congruent addresses.
The patient never developed a specific antibody response to the virus, and the mutations continued using CP.
These findings prompted the researchers to comment, “The therapeutic efficacy of convalescent plasma to date has been disappointing. Its use should be critically evaluated in patients with prolonged viral reproduction. “
This is important because external pressure from specific antibodies leads to selection in a large viral population within a vaccinated patient to an unknown extent. This can lead to escape mutations and viral changes over time, making it more difficult to control the handling and maintenance of the virus.
The researchers also argue that the mutations in the new version B1.1.7 may have appeared in patients with similar disease. Studies like this shed light on the ability to detect the course of viral change during a breast infection to help understand how host factors affect the viral genome. This would be important in the development of both protective and curative agents.
* Important message
medRxiv publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be seen as final, guiding health-related clinical / behavioral practice, or be treated as information established.